COVID-19 is now a worldwide phenomenon - more so than any other event in our lifetime.
These reports examine how the pandemic is impacting CCHF clinics and the people who work in them,
as they live out the gospel among the most marginalized populations in our society.
UPDATES ON LAWNDALE, & PERPETUATING THE PROBLEMS
Here is an update from the Urgent Request I sent yesterday. I had received texts from friends at Lawndale Christian Health Center on Chicago’s west side that “things were starting to get out of hand”. In addition to protests and the violence that has been ancillary to them, rival gangs were at war, taking advantage of a stretched-thin police presence. Geographically, Lawndale’s offices and clinics are on the border of rival gang turf. At the urging of city officials, LCHC closed at 2pm anticipating a major gang attack.
Here is an update from the Urgent Request I sent yesterday. I had received texts from friends at Lawndale Christian Health Center on Chicago’s west side that “things were starting to get out of hand”. In addition to protests and the violence that has been ancillary to them, rival gangs were at war, taking advantage of a stretched-thin police presence. Geographically, Lawndale’s offices and clinics are on the border of rival gang turf. At the urging of city officials, LCHC closed at 2pm anticipating a major gang attack.
Siloam Health in Nashville, TN stopping yesterday afternoon to pray for the folks at Lawndale
News reported that there were 80+ shootings over the weekend, and things were escalating. A doc who has lived in Lawndale over 20 years said that Monday night there was more gunfire, sirens and helicopters than he had ever experienced. Another doc shared that local ERs were more overwhelmed with gunshots and assault wounds than they were with COVID patients at the height of the pandemic. We let you know, and asked you to pray.
Thank you for praying. I received emails and texts from many of you letting me know that you are praying. Clinics stopped in mid-afternoon to gather and pray for protection, peace and healing for our friends and their community. Others mobilized church intercession teams. My staff and Board prayed. Many thousands prayed for Lawndale yesterday. I hope you will continue to pray for Lawndale and other communities like New York, Detroit, Philadelphia, etc. where CCHF clinics are caught in violence. God hears.
The report from Lawndale is that last night was quiet. No riots in the neighborhood. No major gang attacks. No property damage. It was the quietest night they have had in a week. About 4pm yesterday there was a meeting in front of LCHC’s offices between Hispanic and black community leaders, the mayor, and members of the police department. They prayed together and encouraged each other. It was powerful.
Today my inbox has been filled with notes from LCHC staff who are grateful for your prayers. Here is one, thanking me for an email I sent to let LCHC staff know you had prayed for them:
“Your email blessed me so much this morning and welled up my eyes. I needed to send you a note of gratitude. I have lived and worked in Lawndale for over 15 years and the past couple days have been the most intense with just pure utter confusion. The fact that the whole CCHF family prayed for us is very humbling as well as just awesome! …We have such an amazing team here at LCHC but for it to go beyond even our organization to CCHF is so awesome. Days like yesterday I think about calling it quits and taking my family of 6 out of the hood and going to the mountains. So, your note helps me endure.”
Isn’t it crazy that when we feel powerless to do anything, we pray! But prayer is the most extreme, radical, powerful thing that we do. I am an action guy. I pray as a last resort far too often. On June 10 last year I was diagnosed with stage 4 metastatic melanoma. It had spread throughout my chest, lungs, liver, and even included 4 brain tumors. It was aggressive. Prognosis was a matter of weeks or months. In July my oncologist started me on immunotherapy as a last and only option. I had severe auto-immune reactions to the drugs, and they had to stop treatment less than two months in. No treatment. Cancer everywhere. Medically, no hope. But people prayed. Many of you who prayed for Lawndale yesterday prayed for me last year. Six months later CT scans and MRIs showed no signs of cancer. In March, follow up scans confirmed that I was cancer-free – healed with no treatments other than prayer.
So remember these things. Lawndale was at peace last night. I was healed of cancer. You prayed. God heard. Lawndale may blow up tomorrow, and I’ll die of cancer or something else eventually. It still doesn’t change the fact that you prayed and God heard. So keep praying. It is what are supposed to do.
BONUS:
Before I end this note, I want to call myself out for the way the email went out yesterday. One faithful person wrote this back to me after receiving the urgent call to prayer:
“…Are you sure that everyone in these gangs is brown or black? Could you be perpetuating the narrative that minorities are violent? I’m not saying that you shouldn’t ask for prayer or mention the gang activity. I’m asking you to think about why you included the information about black, brown, African American, and Hispanic. I’m wondering if you know you painted a picture of violent black and brown people trapping and frightening presumably white (because you didn’t choose to label them black or brown and it’s not hard to believe that this is what people will picture) people.”
Some of you will read her note and think, “I thought the same thing. I am glad she called Steve out.” Some of you will think, “Lighten up! She is being too sensitive. She missed the point.” So here are a couple of things you should know. First, she prayed for Lawndale, just like we asked. The lady who wrote this is on our side, part of our family, one of us. I am glad she is part of us. We need courageous people like her. Second, I am honored that she shared this with me. It opened a dialogue that needed to happen, and it helped me. She is busy, but she invested valuable time to share with me. I could have dismissed or been offended by it. She took a risk. I think she was gutsy, and I can’t tell you how honored I am that folks are willing to help me this way.
So I should clear up a few things. First, LCHC is not white, and LCHC is not scared. They are back at work today. One of their employees, a black woman, shared that she was caring for a patient who is Hispanic this morning. He was scared and didn’t know how he would be received. She loved him, went out of her way to make him feel secure; and by the end of the visit, he apologized for not hugging her (because of COVID). So LCHC is not scared. And LCHC employs people from the Lawndale community, most of whom are not white. LCHC is an intentionally diverse organization, and much of their staff are black or brown. LCHC is not perfect, and is constantly working on cross-cultural understanding. But diversity is an ingrained value at Lawndale. If you pictured white people being threatened by people of color when you read the email yesterday, ask yourself why. Does that say something about you that needs to change?
Also, I don’t know if everyone in the gangs are black and Hispanic. I repeated what had been said to me by people who live in Lawndale and who are, themselves, people of color. Perpetuating a stereotype was not my intention, but good intentions are not enough. Innocent mistakes still hurt people. We/I have to be careful about the things we say. Please forgive me for that.
The bigger questions we should be asking are “Why are gangs in Lawndale (or ___________ community in your city), and not in Wheaton (or _________ community in your city).” We know the answer to that, and it makes people like me uncomfortable.
I live in one of those under-resourced communities. Before I came to work for CCHF, my wife and I worked with youth in this community. I never met a kid that got into a gang who had other employment choices or role models. I met a bunch of them who tried desperately to stay out of gangs. When you live in a community with people who are different than you, it helps you understand that there are underlying issues driving the brokenness. So here is the offensive statement that you were hoping I would avoid: The systems on which our society is built were designed to benefit the people who made the rules at the expense of the weakest and least powerful. That is almost always meant (I would say always, but I am trying to leave some gap for an exception I have not found yet) white males (like me) created systems to benefit them at the expense of people of color. (Ouch. Truth. Think.) What all the protests are trying to do is to wake up people who look like me to understand the realities that created a system where a policeman can kill a black man in public on film with no fear. The killing of George Floyd is extreme, and we all think it is wrong. But it is symptomatic of a system that has failed most of the people that you and I love and serve.
That is why we are here, and why we do what we do. We are working to create a health system that reflects the society Christ came to inaugurate – the empire/government/society/kingdom of God. When we pray the Lord’s prayer and say “Your kingdom come, your will be done on earth as it is in heaven”, we are committing to order our lives, values and priorities around the idea that if it is not good enough for heaven, it is not good enough for earth. So we sacrificially care for people without consideration of their financial status or skin color. We honor their dignity and see them as our neighbors. We see the image of God in them, and allow Christ to reveal himself to us and meet us through their most broken state. We do this in practical ways, because the kingdom of God is tangible and present, and we are its ambassadors. We will love our brothers, love our neighbors, and love our enemies. We realize we can only do that as we allow the Holy Spirit to transform our hearts and heal our brokenness. Healing and restoration is a progressive thing. When we stop learning, we stop being disciples. Disciples learn, by seeking and following, and allowing ourselves to be challenged. Thank you, sister, for challenging me.
Sorry for the preach. I don’t mean to be intentionally offensive or political. I confess that I am as broken as anyone I know. If you are broken, too, let’s get healed together.
Thanks for praying. Don’t stop.
In Christ’s love,
Steve
A Time To Grow…
I first heard about “Dr. Bob” from a medical student from New York who was doing a rotation in Memphis. She shared about working with Dr. Bob Paeglow at his clinic, and how life-changing that had been for her. “I want to be a doctor like Dr. Bob.” I had never heard of Dr. Bob from Albany, NY, so I looked him up on-line. What I found was a clinic and a doctor who was doing everything CCHF stands for – Christ-centered holistic care, living incarnationally, practicing the 3-Rs, serving those who are poor, living sacrificially. This guy was one of us!
I first heard about “Dr. Bob” from a medical student from New York who was doing a rotation in Memphis. She shared about working with Dr. Bob Paeglow at his clinic, and how life-changing that had been for her. “I want to be a doctor like Dr. Bob.” I had never heard of Dr. Bob from Albany, NY, so I looked him up on-line. What I found was a clinic and a doctor who was doing everything CCHF stands for – Christ-centered holistic care, living incarnationally, practicing the 3-Rs, serving those who are poor, living sacrificially. This guy was one of us!
CBS News and People have done feature articles on Dr. Bob and his work. A few years after I found him on-line, we met when he and his wife, Leane, showed up at a CCHF conference. We have been friends ever since. Bob eventually served on the CCHF Board for five years, has taught workshops at our conferences, and was even a plenary speaker one year. Bob is one of the most generous, sacrificial, convivial, humble and sincere people I have ever known. I imagine that Jesus was a lot like Dr. Bob – deeply spiritual, truly compassionate, and fun at parties.
I had a long talk with Bob last week. The clinic that he founded, Koinonia Primary Care in Albany NY, is doing amazingly well in this COVID season. In order to mitigate the risk of exposure, they have divided staff into two groups that alternate days in clinic and days working from home. They have adjusted to telehealth. They miss being together, but they are taking care of patients, and getting things done. “When patient visits are down, we find other stuff to do. Our clinic has never been as clean as it is now!”
Koinonia is a family. Bob and Leane both work there. Bob’s daughter, Corrie, who has a DPH which has come in handy, is the executive director. Before Corrie, the Paeglow’s son, Bob, Jr. ran the clinic. (Bob, Jr. now works at a CCHF clinic in Raleigh, NC.) The staff have been together for a long time. Koinonia is a family practice that practices family. The staff is “family”, but so are the patients. It is not unusual for them to celebrate patients’ birthdays or milestones, or for Bob to pull out his checkbook to pay for a prescription that his patient can’t afford. While they feel small and intimate, they are incredibly progressive. They have had integrated behavioral health longer than most CCHF clinics. The neighborhood they serve was hit hard by opioid abuse, and Koinonia was one of the first CCHF clinics to start a M.A.T. program. Bob actively mentors students from New York to Texas, runs summer medical projects for students, is involved in CCHF work around the country and overseas work in Africa.
When COVID first hit, Dr. Bob and Corrie made a commitment to not furlough anyone. And they decided they would pay the support staff time and a half for hazard pay. If necessary, they and Leane would take 50% cuts in salary to keep their staff together. But amazingly, they have not only survived without major cuts, they are in better financial shape than they have ever been at this time of the year. They have been able to maintain all of their services, though many are delivered via telehealth. And they have even been able to keep up with their M.A.T. patients.
“God is moving in all this. I think maybe revival is coming. We are being forced out of our molds and routines”
So far Koinonia has not lost any patients. All of their COVID+ patients have survived, though some have been very sick. None of the staff have shown symptoms or tested positive, so they feel pretty good about the precautions they are taking.
The biggest challenge has been to deal with the grief of losing community, both in the workplace and in church life. Bob shared that what has helped him during times when depression was close - a return to life-giving spiritual disciplines. He and Leane have a rich prayer life, and he has been reading 10 chapters per day in the Bible.
New York state has a unique program called Article 28. Becoming an Article 28 clinic allows organizations to benefit from state funded quality incentives as well as other opportunities. Clinics in the CCHF community in New York will tell you that qualifying for Article 28 is more difficult than qualifying for FQHC status. The application is extensive, and for some clinics the process has taken years. Koinonia is not an FQHC, but they are an Article 28 clinic, which has helped.
One of the current programs the state is offering is to financially assist clinics that are adding providers. The state will pay up to $40K in recruitment fees and relocation costs, plus they will reimburse clinics for the first few months until the new providers are able to get up to speed. The program will only be in effect for a few months, so clinics like Koinonia, Beacon (Staten Island) and Jericho Road (Buffalo) are eager to take advantage. All of those clinics are looking for medical and behavioral health providers.
They would be hiring providers even if the New York program were not in place. And they are not alone. As I have interviewed clinics across the country, all of them are hiring. ALL of them. I have never seen such a demand for missionally-minded providers in my 12+ years in CCHF. Everyone is in growth-mode. The biggest need seems to be physicians and psychologists. But almost everyone is looking for mid-levels and LCSWs, too. Some clinics are hiring at every level – dental, pharmacy, executives, etc.
What to make of this unexpected season of growth in virtually every region of the country, urban and rural, east, west and all in between? I have a hunch, but I will hold that for now.
“God is moving in all this.” Dr. Bob said, “I think maybe revival is coming. We are being forced out of our molds and routines. We all felt so confident and secure, and then a microscopic virus toppled everything. We are learning new ways. This whole thing has taught us how to reach this generation, this culture. Some of us old guys didn’t like or want to understand technology, but now we are all doing it, and we found that we can. I think that is a good thing.”
Bob and I talked about how virtual church services are reaching more people than ever, but they don’t know how or why. That is true, even of these CCHF Special Reports. Stats show that about 3,000 people who we send these to will open and read them. But we also know that over 8,000 unique people have read them. There are not 8,000 people in the CCHF database, so some of you are reading these reports and sharing them. Most of the people who read these reports are not in our database. We don’t know who they are or how they found us.
Churches offering on-line services are experiencing the same thing. This phenomenon is not reflective of the quality of their on-line productions, or of our Special Reports. It does tell us that there is a spiritual hunger that much greater that we realized. People are looking and asking questions. They are seeking, on their own initiative.
We have seen this by experience for years. In clinic it is rare for a patient to refuse prayer, or to say that they are uncomfortable talking with their provider about spiritual health. Providers who regularly pray for their patients will tell you that it is more common for patients to insist that they pray for them than to ask them not to. And this is true regardless of where you practice. It doesn’t matter whether you are in Tulsa or Albany, New York, cities that represent both ends of the religious/secular spectrum. There is a spiritual hunger in people, and it is bigger than we think.
“If COVID has taught us anything, it is that we are not as indestructible as we think we are. I hope it is showing all of us that we need God.” Bob is praying that God will find he and his staff ready. They are praying like Jesus told the disciples to when he saw brokenness, chaos, isolation and oppression. “Pray earnestly for the Lord of the harvest to send laborers into the field. The harvest is plentiful, but the workers are few.”
P.S. – If you know someone who wants to use their medical talents to serve Christ by serving the poor…not just a Christian doctor who wants to work with other Christian doctors, but someone who is willing for God to use them in difficult places with difficult people dealing with co-morbidities that they might see in a 3rd world country… if they want to be a doctor like Dr. Bob, I want to know them, too. Give them my name and email.
In Christ’s love,
Steve
A PEAK BEHIND THE CURTAIN
It has been inspiring to report on what folks in our CCHF family have been doing, and how they have been affected by the COVID crisis. I thought this morning I would share how the CCHF staff is doing, and how COVID had impacted us.
We are all well. We watched COVID progress, and like many of you were unsure how to deal with it until mid-March. We decided to cancel the conference just two weeks before it was scheduled, and we started working from home. Because two of us are considered “high risk”, and we share offices space with a large health center, we will continue to work from home until sometime this summer.
It has been inspiring to report on what folks in our CCHF family have been doing, and how they have been affected by the COVID crisis. I thought this morning I would share how the CCHF staff is doing, and how COVID had impacted us.
We are all well. We watched COVID progress, and like many of you were unsure how to deal with it until mid-March. We decided to cancel the conference just two weeks before it was scheduled, and we started working from home. Because two of us are considered “high risk”, and we share offices space with a large health center, we will continue to work from home until sometime this summer.
“Nobody’s ship is sinking, but in this crisis, folks are eager to know how everyone else is doing. The answer: Better than you expect. Why? Because God really is with us. ”
Early on we set some priorities, and have been working through those. First, we determined to survive this crisis by staying healthy and figuring out how to make it financially. Our conference makes up 50% of our annual revenue, so that presented a real challenge. More on that later.
We have been praying for and staying in touch with people in the CCHF community, listening to understand what they need during this time. And what they need right now is a break. People need short bits of time to reflect and process and talk about their experiences. They need connection with others, affirmation, and they need reminding that God is with them. This is an over-dramatic illustration, but it feels like when a ship suddenly sinks. Everyone is in the water, and the first thing they want to do is see who else made it off the ship, find them, and cling together. Nobody’s ship is sinking, but in this crisis, folks are eager to know how everyone else is doing. The answer: Better than you expect. Why? Because God really is with us.
We are also using this time to think through what the world is going to be like post-COVID. When I came to CCHF over 12 years ago, I knew nothing about healthcare. Everything I know I have learned from you. I knew very little about CCHF. I knew that CCHF was an amazing and historically significant organization, and that it needed a reboot. So we tried to be faithful to the values and mission that form the roots of CCHF: commitment to the gospel as God’s total answer to man’s total need, responsible and radical response to brokenness and injustice in healthcare, love expressed through personal sacrifice, and intentionality in the way we practice, the places we live and engage, and in keeping Christ at the center of all we do. And we rebuilt CCHF around the needs of the CCHF community at that time.
“The world has changed in the past 13 years, and so has our community. And it is changing even more through this worldwide crisis. Perhaps this is a time to make some adjustments as an organization.”
The world has changed in the past 13 years, and so has our community. And it is changing even more through this worldwide crisis. Perhaps this is a time to make some adjustments as an organization. (I am not leaving, so get that out of your minds.) I’ll bet the organization you work for or lead is going to look different, too.
Dietrich Bonhoeffer, author and activist, is a great inspiration to me. In letters that he wrote to a friend while in a Nazi prison camp during WWII, he talked about his concerns that Christianity had become a religion content with answering questions that fewer and fewer people were asking. He felt that Christians had allowed Christ, the ultimate Truth, to become merely the answer to the unanswerable. In an age when science offered reasonable explanations for many of the “big questions”, Bonhoeffer challenged us to recover “God in the midst of life” as opposed to God outside the margins of our understanding. He urged our generation to hold on to the ancient truths, but to find new languages to help us speak relevantly into an increasingly religious-less society. This challenge to relevancy has been a driver for me.
“Certainly the sovereign LORD does nothing without first revealing his plan to his servants, the prophets.”
During this season of dramatic change, we can either be resisters, followers or innovators. But change is coming, and God is in it. If God is indeed working in some accelerated way, there are two things I should do now. The first is to rededicate myself to him, making sure that all I have and all I hold dear are on the altar for him to do with as he pleases. Rededication is a good first step. The second is to be a seeker…to read and pray, to be observant, to ask questions, to watch and listen and muse. Amos 3:7 says, “Certainly the sovereign LORD does nothing without first revealing his plan to his servants, the prophets.” I may not be a prophet, but I am part of God’s prophetic community. I doubt that what God is doing is any different than what he has always been doing; but the speed and the way he is doing it may be different that I am used to. So I am using this time make sure that I am aligned with him and to seek.
Here is a quick personal update on each of the CCHF staff. These are faithful people who really do pray for you and who care deeply about being an encouragement and support to this movement:
Tia
(communications)
Tia is stepping away from CCHF to homeschool her 3 children and support the work that her husband has been doing as a family physician and in their community. She was able to help care for a missionary friend who was separated from her family for over a month due to COVID related travel restrictions and now is helping that reunited family as they settle in for a few months.
Angela
(in charge of our placement efforts)
Angela has been sharing work-at-home space with her husband, who is a teacher and coach at a nearby prep school. Angela’s oldest son along with his wife and two young boys moved in for four months after the rapid sale of their home and delayed construction of their new home. With frequent visits from her other adult sons and daughter they have a full house!
Jessie
(heads up our student work)
Jessie and her husband live in Jellico, TN, deep in Appalachia. Jessie has always worked from home, so this is not new to her. Her house is full of family (some recent changes due to COVID:19). They are having church at home now as well. In mid-March Jessie finished up a mission trip to Clarkston Georgia where she spoke at the Emory medical campus and Philadelphia College of Medicine Campus – CMDA groups. She is so glad that happened before everything shut down!
Jason
(graphics, strategies and communications)
Jason lives in Knoxville, and is also a work-from-home veteran. His wife delivered a baby boy during our first week of quarantine. Jason’s siblings and their families are all overseas missions workers, who have returned to the states because of COVID related issues. Jason is busy with Special Reports and strategic issues, plus he is working with several CCHF clinics to help them with websites and various graphic projects.
Sarah
(a new “re-addition”)
Sarah worked for CCHF until she and her husband headed overseas to do work in a closed country several years ago. COVID has made things difficult for many missional workers, especially in parts of the world where there is a mistrust of foreigners. She and her family will be in Memphis for a few months, and we are glad to have her back as part of our team.
Kristy
(chief of all things)
Kristy keeps up with all of us, helping us all stay in touch and on track. Her husband has always had a home office/studio. Finding spaces, times and distance has been a fun challenge most days. Kristy, a coffee snob, says that she enjoys working close to her coffee pot; but she misses the easy rhythms of our work when we are together… and having a reason to accessorize. ☺
Steve
(alias “Big Kahuna”)
I work from a spare bedroom with a TV tray as my desk. I spend about 40% of my time on the phone. My wife, Victoria, retired last year. We are helping care for our 7-year old granddaughter whose mother coordinates drive-thru testing centers for a large health center. Vic recently fell and broke her dominant arm, so I am learning to cook for the first time in my life. So far so good. (Thank God for YouTube.)
John Perkins
John is not on CCHF staff, but he is our founder and we stay in touch. John has been battling cancer found in his colon, and spent the first part of the year recovering from surgery. He is working on yet another book. Next month he and Vera Mae will celebrate their 70th anniversary. Two days later he will turn 90.
Regarding the loss of the conference and its financial impact on CCHF, over half of the folks who had paid for their conference registration opted to donate that to CCHF as a gift. And all of the organizations who had given sponsorships for the conference also allowed us to keep those as contributions to CCHF. The result is that we are able to move forward. We still have needs, but we are not worried about survival. We are humbled that at a time when everyone is hurting, people have been so generous. It reminds us that God is with us, too.
If you are reading this on Friday, CCHF has a big Board Meeting on Saturday. Please pray for us as we recognize what God has done, and look ahead to how we can best help this movement grow in strength, influence and faithfulness.
This is a great community.
In Christ’s love,
Steve
Integrated Care in a Telehealth World
The move toward integrated care and patient centered medical home models has not been an easy transition in most places. PCMH, on its best day, sees PCPs, BH providers, spiritual care workers, social workers and case managers working as a team to help patients manage chronic conditions and move towards a full healthy life. Experience has proven that having all those varied disciplines share spaces, being within eye-shot of one another, is an important key to making the model work.
In the past two months, most clinics have converted >50% of their patient visits to telehealth. Social workers, case managers and BH providers are mostly working from home. I was curious to find if integrated care is another casualty of COVID-19. So I talked with T.K. Brasted, Behavioral Health Director at Hope Central in Seattle, Casey Clardy, Director of Behavioral Health at Lawndale Christian Health Center in Chicago, and Jesse Malott, Behavioral Health Director for Christ Community Health Services in Memphis.
The move toward integrated care and patient centered medical home models has not been an easy transition in most places. PCMH, on its best day, sees PCPs, BH providers, spiritual care workers, social workers and case managers working as a team to help patients manage chronic conditions and move towards a full healthy life. Experience has proven that having all those varied disciplines share spaces, being within eye-shot of one another, is an important key to making the model work.
In the past two months, most clinics have converted >50% of their patient visits to telehealth. Social workers, case managers and BH providers are mostly working from home. I was curious to find if integrated care is another casualty of COVID-19. So I talked with T.K. Brasted, Behavioral Health Director at Hope Central in Seattle, Casey Clardy, Director of Behavioral Health at Lawndale Christian Health Center in Chicago, and Jesse Malott, Behavioral Health Director for Christ Community Health Services in Memphis.
You might ask why CCHF, whose mantra is “living out the gospel through healthcare among those who are poor”, is concerned about integrated care models. We believe that whole person care is essential to the gospel. The gospel as Jesus lived it out, is a whole-person gospel. He cared for bodies and souls – for individuals and their social systems. He healed the sick, and taught us how to love one another in practical world-changing ways. A biblical view of life and health includes spirituality, physiology, relationships and social constructs. God reconciles individuals, ethnos and the cosmos to himself; and he has entrusted the ministry of reconciliation to us. So any view of health that is purely spiritual, without addressing our bodies or our engagement with the world around us is sub-biblical. So is any approach that addresses physiology without addressing spiritual health, mental health and relational health. As health ministries grow, they should grow towards a holistic approach that addresses the whole person.
So how is integrated health being walked out at a time when we are suddenly all doing tele-medicine? The good news is that it is happening. And there are a number of reasons why.
First, PCPs realize the value of working more closely with behavioral health providers, social workers and case managers. Physicians have always been the gatekeepers to care, and for good reason. Without their initiation, there are no warm handoffs. That is still true. But “the warm hand-off” is no longer a new concept in most places. Where there has been a history of integrated health, PCPs are eager to see it continue, and they are helping make that happen.
Secondly, this pandemic has raised the need for behavioral health. It is undeniable. Hypertension, strokes and heart attacks are on the rise. Social media and the news subject us to projectile agoraphobia. Many are facing devastating issues like the loss of friends, family, and jobs at a time when the resources that we normally use to cope are unavailable. Children with special needs are unable to access the resources on which they and their families have come to depend, and the effect on both child and parent is overwhelming. Acts of racism and domestic violence are on the rise. Isolation makes it difficult for victims of abuse to escape. People feel trapped in ways that often lead to unhealthy mental states. Anxiety and depression are a greater pandemic than COVID-19.
Third, care teams know that their most at-risk patients face particular challenges. Patients with bi-polar disorders, OCD, schizophrenia, and other disorders who depend on regular medication, stable routines, and consistent visits to their doctors and counselors are dealing with major interruptions. And these are people who don’t handle interruptions well. Many organizations have temporarily closed satellite clinics. Without providers and care teams being proactive, some of those patients will inevitably fall through the cracks. One psychologist told me that her group has 60 patients on long-term meds who need monthly injections. Many of those have moved or gone underground during the COVID crisis, and have lost their connection with their BH providers and PCPs. For those patients, telehealth doesn’t work.
“We love being present with our patients. Presence is our most powerful tool. With COVID, we are reduced to a two-dimensional encounter with a lot of our patients”
Primary care physicians see and understand these needs, and are eager to engage members of care teams in addressing mental, social and spiritual health in their patients. Where they can, they attempt to provide preemptive care for patients who are at highest risk. Having a social worker or psychologist call to check on a patient, or asking a case worker or spiritual care provider to phone a patient who is facing crippling hardships...with all of its challenges, COVID is an ideal place for integrated health to shine.
In addition to patients’ needs, there is a daily need for staff care. Dr. Clardy told me that 85% of Lawndale staff are not working where they normally work. That is true in many clinics. People are having to adapt to different tasks in different places during this extended crisis. PCPs are often put in the position of providing care for someone else’s patients. It’s not ideal, but it is necessary, and adds to the stress load for providers who normally care for established patient panels and usually see one or two new patients per week.
I asked Jesse Malott why everyone is so tired. “You know, I think a big reason is that we are all exercising unused muscles. Behavioral health folks, and really all primary care providers, chose to do what we do in part because we thrive on presence. We love being present with our patients. Presence is our most powerful tool. With COVID, we are reduced to a two-dimensional encounter with a lot of our patients. Being on a screen all day long is exhausting, partly because we are having to use different ways than we are used to in order to establish empathy and to provide effective care.”
Casey shared, “Providers and case workers are learning to do things they haven’t been trained to do, or at least have not done at this level. And they are doing it at a time when we are having to be proactive with so many patients. Providing care, making decisions, and learning new processes on the fly is hard for staff. Layer into that the amount of loss and grief that we confront daily. We are all feeling slammed. COVID seems to magnify dysfunction. The staff needs care from us as much as the patients do. They need time to process the anxiety, imbalance and grief that they take on every day, not to mention their own.”
So how are folks doing integrated care during a time when we are often not co-located and when we are seeing patients on a computer screen or smart phone? Here are some things that Casey, Jesse and TK shared with me:
Behavioral health providers and other care team members have to flex and mold to and around the medical provider. They have to be flexible and find their way into this new model of delivery. They have more flexibility than PCPs, so they need to take this on.
Care team members working off-site should be proactive by calling in for staff devotions and participating in staff briefings.
BH providers can text PCPs to let them know when they have a no-show and are available to “step in” to a visit. They should keep their phones open for texts from PCPs.
BH providers should utilize some time to provide pre-emptive coping strategies via FB or ZOOM group meetings. They can guide PCPs and other care team members in patient education efforts, virtual group meetings and resource sharing.
In larger organizations with multiple BH providers, IT departments can set up a BH portal that allows PCPs to text during tele-med visits so that any available BH provider can respond and facilitate a warm tele-hand-off. Where this has been implemented, it has reduced warm-hand-off-no-shows (won’t-waits). The number of “won’t-wait” patients on telehealth visits is much lower than those in clinic.
There have been positives in telehealth visits by behavioral health and case management staff. It often provides an opportunity to virtually visit the patient’s daily environment. Everyone has a story about getting to virtually meet family members and positively engage in the patient’s support community. It is nice for providers to get to see patients in their natural habitat. Another positive is that while medical and dental visits are down, behavioral health visits are up in most of the clinics I’ve talked to.
The move to telehealth has exposed further barriers to care for the populations we serve. In cities like Memphis, 70% of homes in low income neighborhoods do not have reliable internet connections. In places where government insurance will not reimburse non-video behavioral tele-health visits, that is a problem.
I am always interested to hear what you are doing to make integrated health work. Leave comments in the space below, or drop me an email and let us know how it is working for you.
Thank you for all that you are doing – working those unused muscles – to extend Christ’s love to marginalized people, and being living examples of gospel of reconciliation through Christ. We are praying for you.
In Christ’s love,
Steve
THOSE WHO ARE UNHOUSED
I had to make a pharmacy run this morning, and noticed some new faces on street corners in a part of town where it is rare to see homeless people. It made me wonder, “Is the number of people experiencing homelessness increasing, or is this a consequence of social distancing in shelters where unhoused folks usually stay.”
I called Bobby Watts, CEO for The National Health Care for the Homeless Council. NHCHC works with clinics, Christian and secular, that serve as service providers in shelters around the country. Many CCHF clinics are also connected with Bobby and the Council. Bobby told me, “Yes, all the projections are that homelessness is on the rise, but it is hard to document due to this unusual situation.”
I had to make a pharmacy run this morning, and noticed some new faces on street corners in a part of town where it is rare to see homeless people. It made me wonder, “Is the number of people experiencing homelessness increasing, or is this a consequence of social distancing in shelters where unhoused folks usually stay.”
Bobby Watts, CEO
National Health Care for the Homeless Council.
I called Bobby Watts, CEO for The National Health Care for the Homeless Council. NHCHC works with clinics, Christian and secular, that serve as service providers in shelters around the country. Many CCHF clinics are also connected with Bobby and the Council. Bobby told me, “Yes, all the projections are that homelessness is on the rise, but it is hard to document due to this unusual situation.”
Shelters as well as local and state governments are responding to this crisis in varied ways. While many shelters are unable to easily restructure spaces to accommodate social distancing, others have increased empty spaces, which has led to reduced capacity and more people on the streets. Some cities and states have set up temporary shelters in sports arenas, conference centers, warehouses, armories or hotels to reduce population density in shelters. Many of those are run by hospitals, health departments, or even the military. This pandemic hit the U.S. during temperate weather months; and so many of the usual shelter utilizers have chosen to remain outside. All of this makes tracking growth in the homeless community almost impossible. But homelessness has clearly increased.
“Yes, all the projections are that homelessness is on the rise, but it is hard to document due to this unusual situation.”
One outcome of COVID-19 is that many missions and shelters are designing spaces that will allow for social distancing in the future.
There have been significant changes in homelessness, and some of those could be long-term.
Unemployment has not only meant a loss of income, but also a loss of health benefits for tens of millions. The leading cause of bankruptcy over the past 40 years has been medical expenses.
It is estimated that 20% to 40% of those experiencing homelessness were employed before the COVID-19 recession. People who were beginning to climb out of homelessness through recent employment, those who have no margin yet, were the first to be laid off as the economy shut down. They will almost certainly slip back into homelessness.
Many who were staying with friends or relatives lost that option due to fears of spreading the virus to or from their hosts.
All of these factors point to an increase in homelessness. A local administrator for a homeless shelter in my city is seeing an increase in the number of homeless men from out of state. One cause could be the loss of shelter in small towns in our tri-state area. Whatever the reason, these are strangers searching for resources in new places, and they present a danger of disease transmission as they travel.
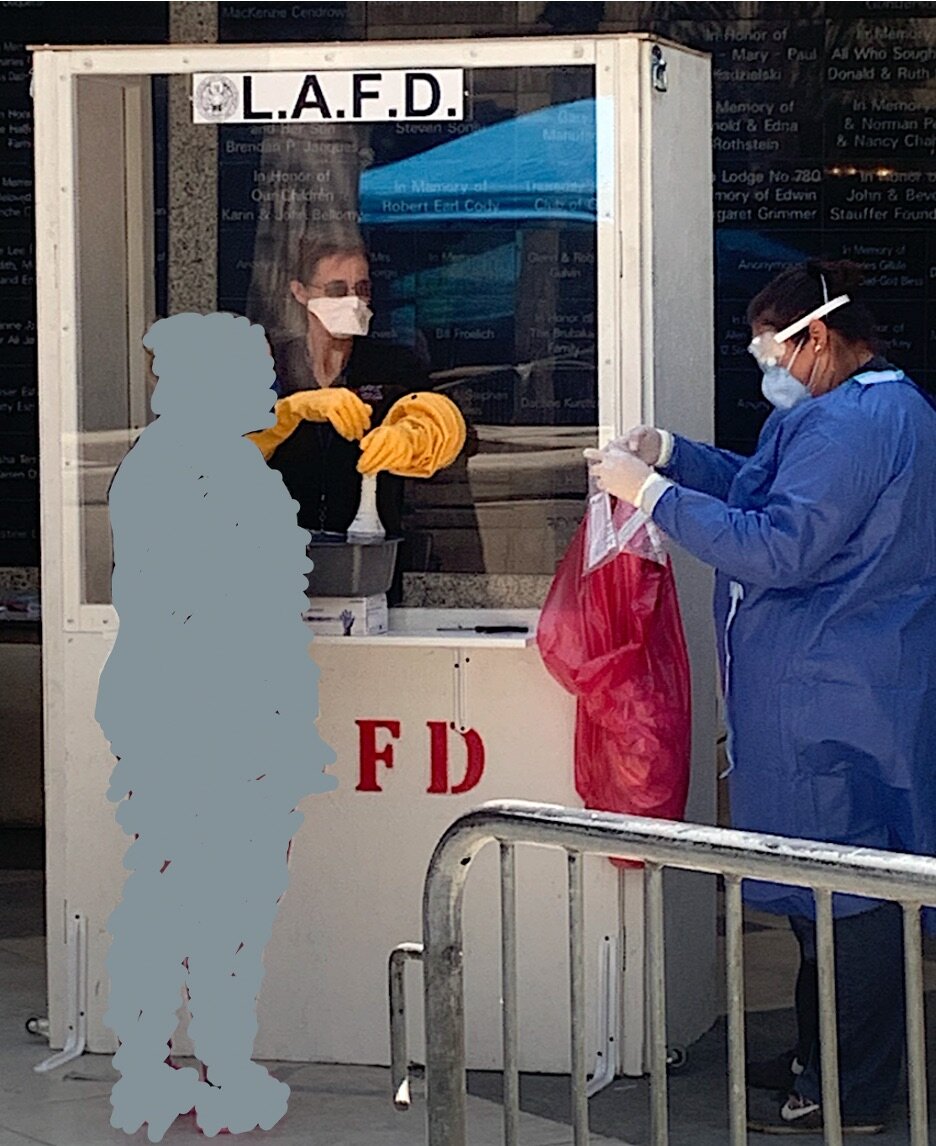
Dr. Katy White, CMO
LA Christian Health Center
Most of the places I have interviewed say the number of COVID+ is small in their homeless communities. One of the larger missions in Memphis has only had one COVID+ guest, a new arrival who was infected in the local jail from which he had just been released. I spoke with Dr. Katy White at LA Christian Health Center. In the past 10 days they have done mass testing at several of the large homeless shelters on Skid Row. There appears to be the beginning of an outbreak in one of the shelters, and they are working to contain that. But other shelters have had very few guests or staff test positive. The same is true for street testing on Skid Row. City Gate Network (formerly the Association of Gospel Rescue Missions) reports that in most places the greater risk is for homeless guests to be infected by volunteers and staff, not the other way around. A number of shelters, like one in my city, have temporarily suspended having volunteers in the shelters in order to protect their guests and staff.
But that is not true everywhere. Some shelters in Boston have an infection rate of over 50%. Similar numbers were found in Chicago in places like the Pacific Garden Mission. Bobby Watts and NHCHC have been working with the CDC to develop guidelines that call for mass testing for all shelters and encampments. When an outbreak happens, it happens quickly.
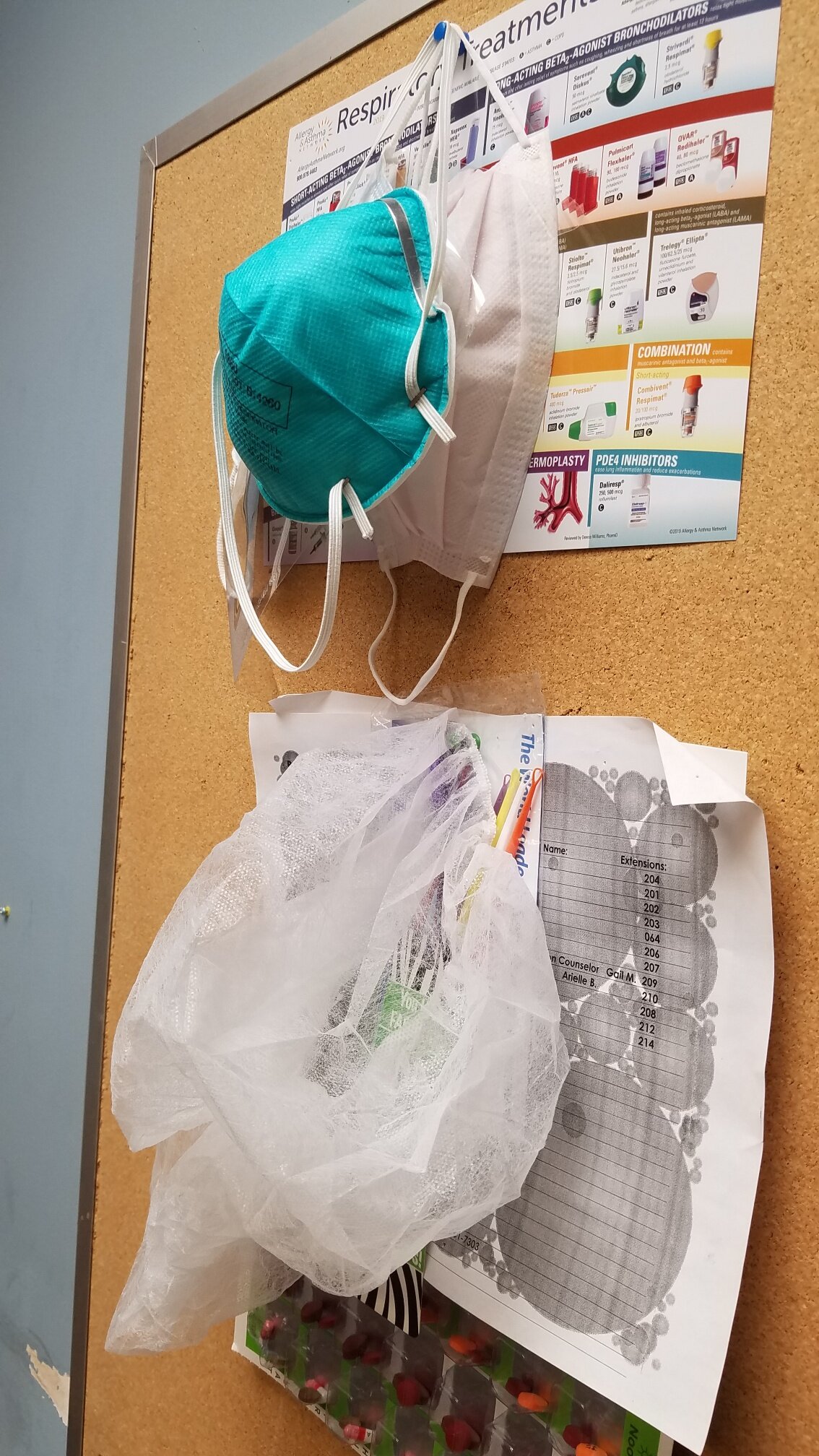
Where infection rates are low, the typical strategy centers around sanitizing, providing gloves and masks, encouraging social distancing, and isolating COVID+ patients. Their testing and screening is targeted on staff and new guests. But where infection rates are high, or in high density areas like Skid Row or San Francisco’s Tenderloin district, the strategy is to isolate high risk, non-positive people.
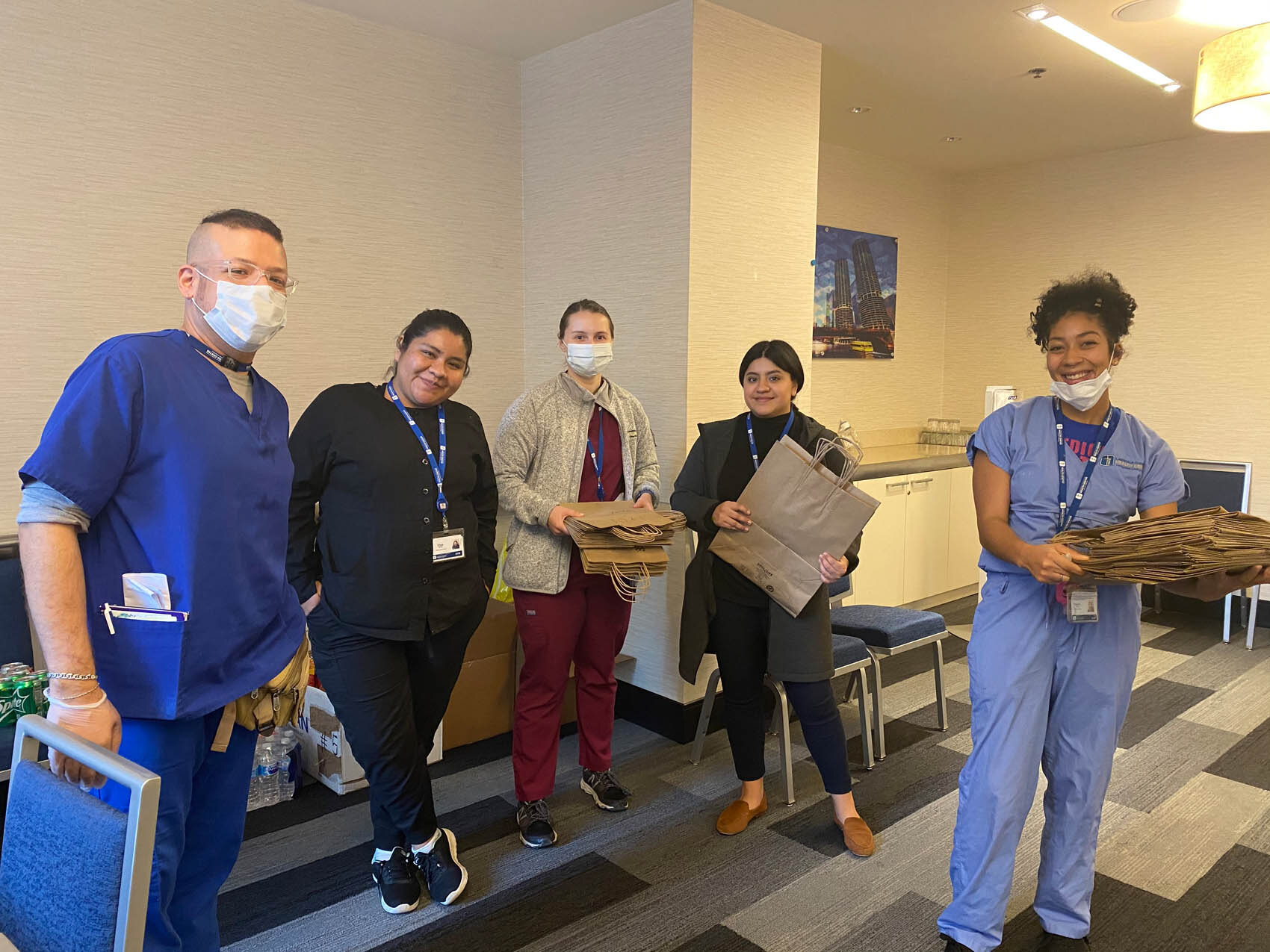
In Chicago, our friends at Lawndale, in partnership with the Cook County health department, started isolating COVID+ unhoused people in a downtown hotel. But when the infection rate exploded at some of the large shelters, their strategy shifted to identifying elderly patients and those with co-morbidities that make them high risk, and isolating them in a hotel to keep them safe. It has been an amazing feat. Lawndale staff are not only providing medical and spiritual care, but are providing “room service” (meal delivery), cleaning, sanitizing, and some programming to the guests there. It requires round-the-clock staffing, and a different management structure and skill set than they are used to. But they have risen to it, and are helping other clinics figure it out in other cities. (Here is a link to a story in the Wall Street Journal about what Lawndale is doing.)
Dr. Katy White told me this week that they are working collaboratively to not only do mass testing in the local shelters, but also to identify high-risk homeless neighbors. They are in the process of moving 15,000 high-risk patients to hotels around the city, and will be managing medical care for those with chronic diseases. They are adding temporary medical staff for this, and are hopeful that medical missionaries on unscheduled furlough might join them in this effort.
At Water Street Mission in Lancaster, PA, the infection rate has been low, but they have had a couple of serious cases. Two of their guests are currently in ICU. Greg Kessler, the VP of Health Services at Water Street, wrote me this afternoon asking for prayer for them and for a staff member who is recovering from COVID at home.
Greg Kessler, VP of Health Services Water Street Mission
One popular strategy in large municipalities is to create Alternate Care Sites, or ACSs. ACSs are an attempt by local governments to provide temporary housing for homeless populations during this time of social distancing. Some have moved homeless patients into RVs located in closed state parks. That has not always worked well because many are afraid to be moved to remote places where they have no community or familiar resources. Others create ACSs in conference centers and hotels like they are doing in Chicago and Los Angeles. That is often met with resistance from non-homeless people, fearful of having sick homeless people in their communities, or afraid that they won’t leave when this is over. In places like Ohio and Pennsylvania, the national guard has been used to help set up and staff ACSs. While well intentioned, there is concern that military or police presence makes guests feel more like prisoners. For those whose lives have been characterized by severe trauma, this can aggravate anxieties, and exacerbate fears and irrational behavior.
Some of us are in positions of influence, and have a voice into government agencies and task forces. One way we can help is to advocate for ACSs to embrace trauma-informed policies and programing that help those in temporary housing to live in peace and dignity.
Organizations like City Gate and the National Health Care for the Homeless Council have a broader perspective on these issues, and can help us use our influence wisely. Bobby Watts (NHCHC) and John Ashmen (CEO for Citygate Network) are leaders who love Jesus and who love those experiencing homelessness, and can counsel us as we serve the most vulnerable in our communities.
In Christ’s love,
Steve
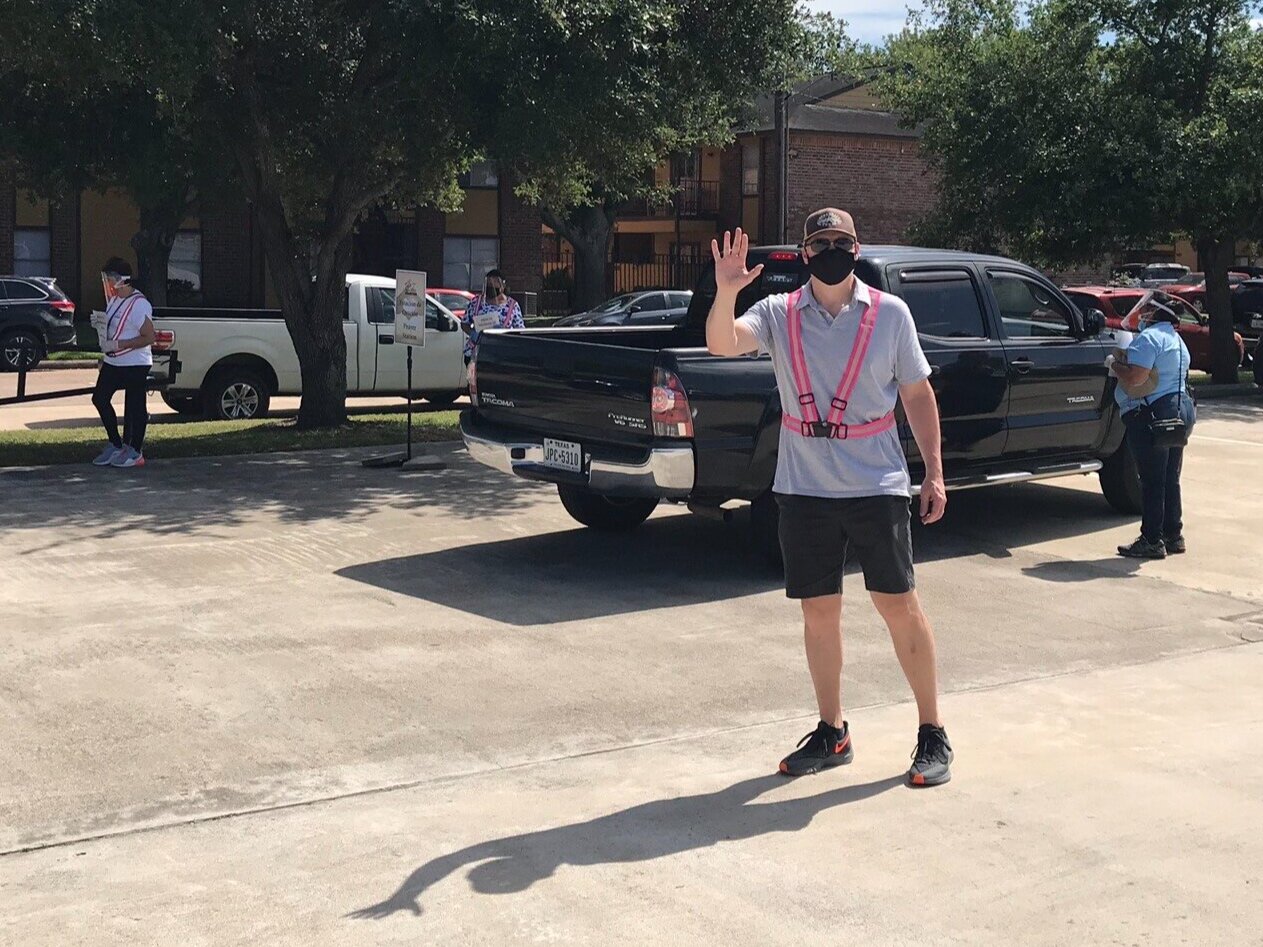
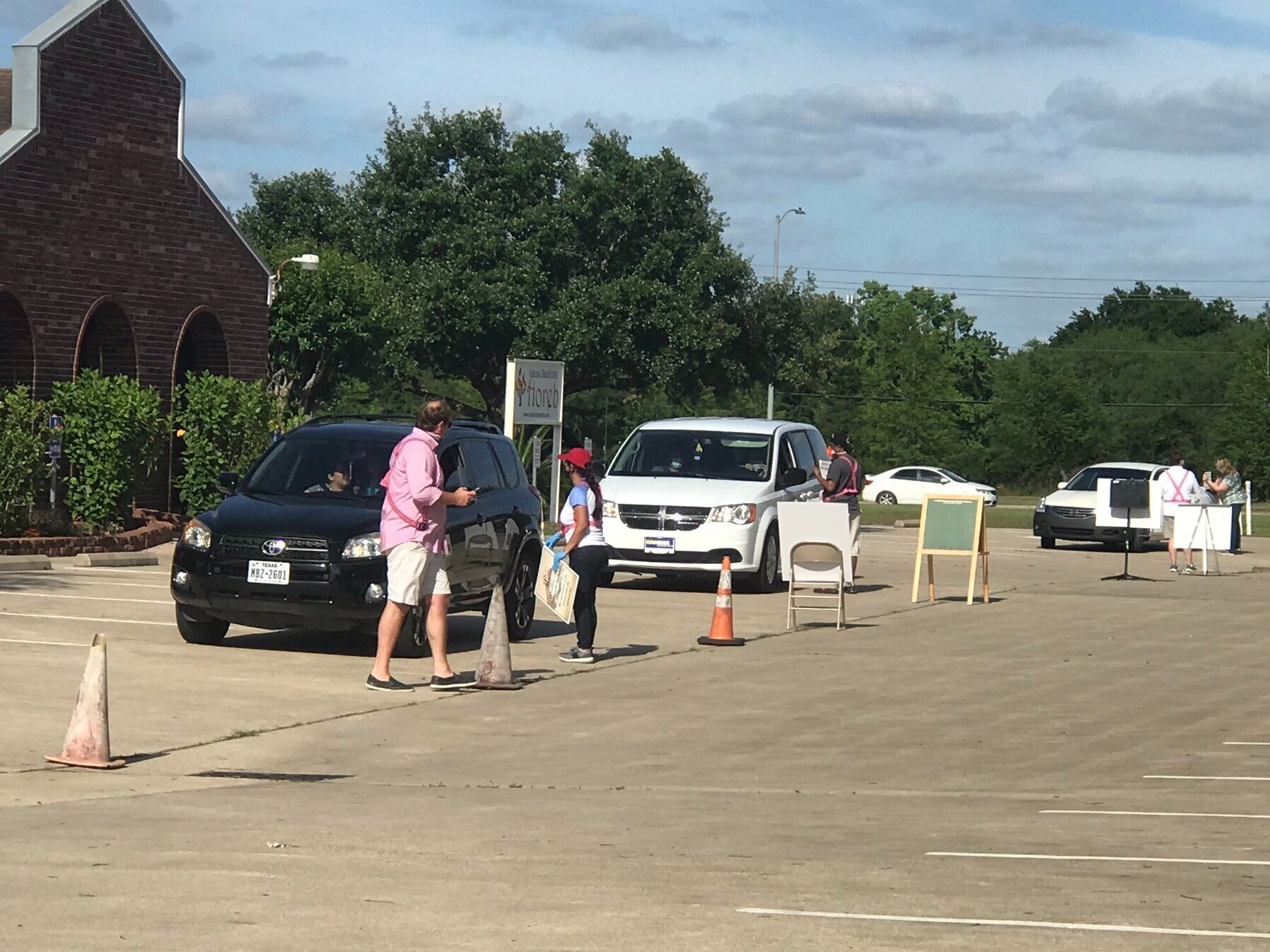
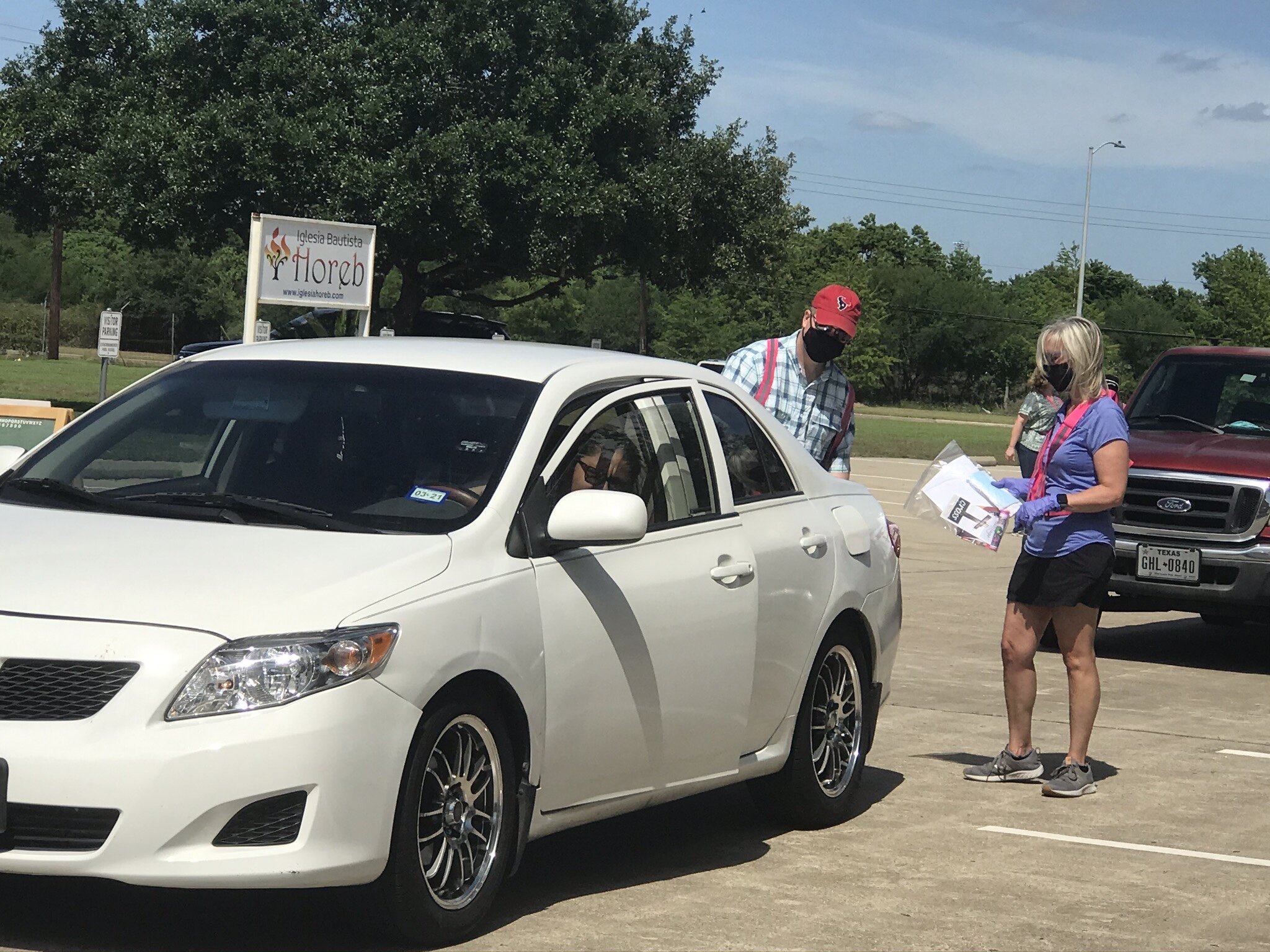
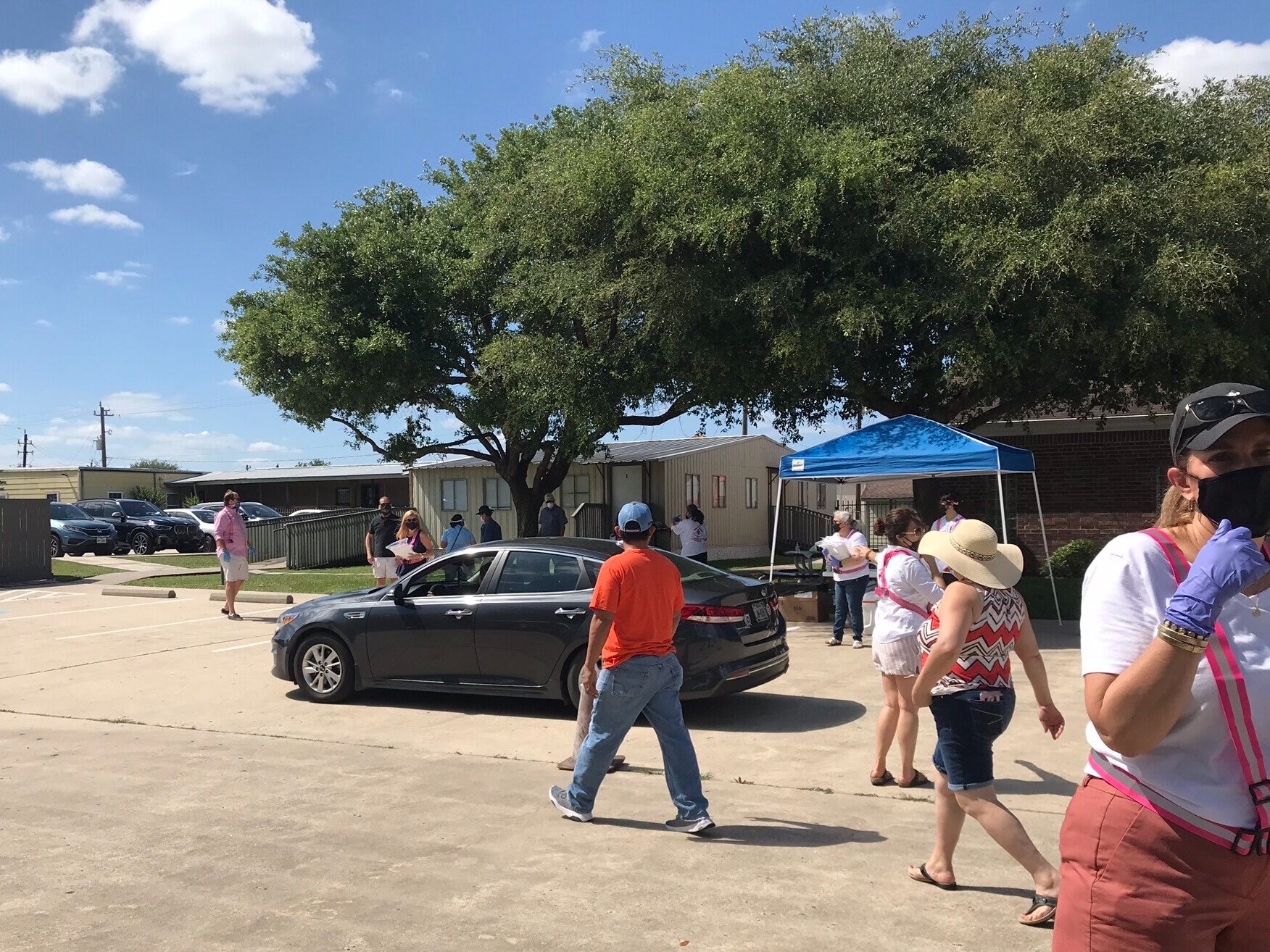
NOT AS UNPREPARED AS YOU THINK
Almost every clinic leader I speak to has a story about how God began preparing their organization for this pandemic long before they ever heard of COVID-19. Julissa Chappell is the executive director for Casa El Buen Samaritano, a charitable clinic in southwest Houston. As you might have guessed by the name, Casa exists to serve a community of mostly non-English speaking immigrants, all of whom are uninsured and earn less than 200% of the FPL. For the past 10 years they have been open two afternoon/evenings each week, which is the best time for their patients to visit. Their provider staff were mostly volunteers, supported by a few full-time administrative staff and several part-time medical assistants and spiritual care providers. While some free/charitable clinics have temporarily stopped seeing patients, this has been a season of growth for Casa.
Julissa Chappell
Almost every clinic leader I speak to has a story about how God began preparing their organization for this pandemic long before they ever heard of COVID-19. Julissa Chappell is the executive director for Casa El Buen Samaritano, a charitable clinic in southwest Houston. As you might have guessed by the name, Casa exists to serve a community of mostly non-English speaking immigrants, all of whom are uninsured and earn less than 200% of the FPL. For the past 10 years they have been open two afternoon/evenings each week, which is the best time for their patients to visit. Their provider staff were mostly volunteers, supported by a few full-time administrative staff and several part-time medical assistants and spiritual care providers. While some free/charitable clinics have temporarily stopped seeing patients, this has been a season of growth for Casa.
Bailey Monarch
Early this year, Casa held their annual fundraising banquet. They were blessed with generosity exceeding all of their previous events. The influx of cash allowed them to finish their IT overhaul, which began 2 years ago after Hurricane Harvey. Within a couple of weeks, after a year of searching, they hired a new provider, Bailey Monarch. Bailey is a nurse practitioner who trained and worked at a large Christian clinic in Memphis (CCHS) before moving to Houston last fall to get married. Bailey loved her time in Memphis, and worked in an environment where she prayed and shared with her patients. When it was time to move to Houston, she contacted Angela Counce at CCHF|Match, and Angela directed her to Casa El Buen Samaritano. Bailey not only brought her skills as an NP, but understood the culture and mission at Casa. Due to the skill set and contacts she brought from her time in Memphis, when the shelter-in-place order hit, Bailey was able to help Casa set up their tele-health program.
When the city shut down, Casa remained open during normal clinic hours, but face-to-face visits are down just like everywhere else. However, they were able to shift to tele-health without sacrificing quality of care or the spiritual health that their patients have come to appreciate. Their spiritual health staff are also trained in community health, so they decided to proactively telephone patients with chronic conditions (hypertension, diabetes, hyperlipidemia and women’s health). That allowed them to address anxieties in their patients, minister peace, and help their patients adopt good practices that have kept them well. As far as they are aware, none of their patients have contracted COVID-19. Casa has doubled their days of patient care, picked up new patients, and maintained personal touch with old patients, directing them to Christ through prayer. All this was made possible because God provided the funds to complete their IT overhaul and to hire Bailey just before COVID-19 rocked everyone’s world.
Christy Chermak
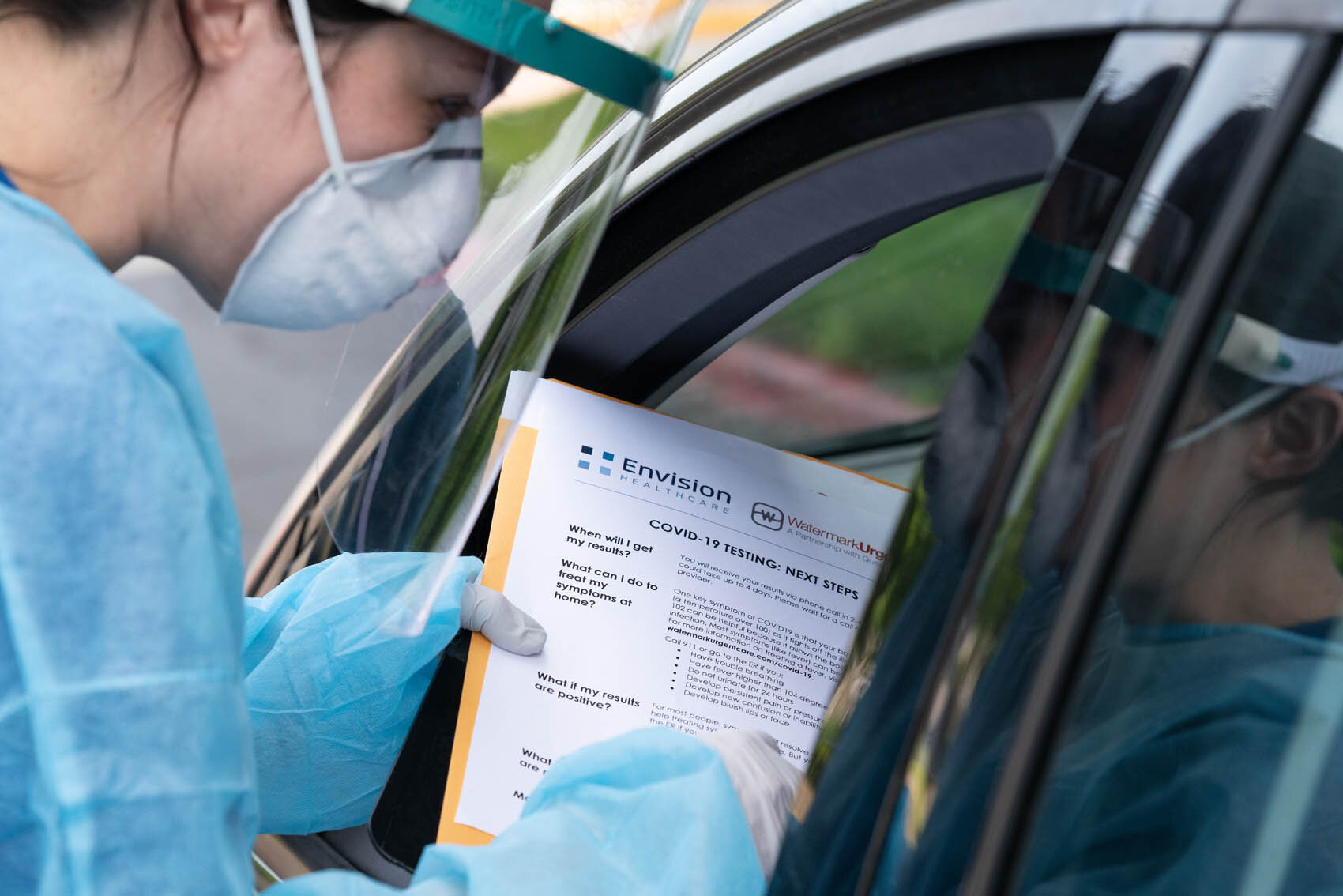
Christy Chermak oversees Watermark Health, a ministry of Watermark Community Church that includes two urgent care clinics on the north side of Dallas. In 2014, not long after Watermark opened their first clinics, Dallas was shaken by the Ebola crisis. In addition to a huge medical community, Dallas is a major refugee resettlement area, and many of the neighborhoods where refugees live are on the north side. Watermark remembers how the Ebola crisis raised the level of anxiety in both refugee and medical communities, and what some of the long-term impact was from that. While their clinic staff is relatively small, they utilize over 200 volunteers, including many medical providers who work in ERs, ICUs and on ambulances when they are not volunteering at one of the clinics.
Not surprisingly, patient visits dropped off at the Watermark clinics; and temporarily, so did the need for volunteers. But Christy felt that the capacity they now had due to lower patient volume could be filled by ministering to staff and volunteers. “We know medical professionals can lend towards compartmentalizing and over time becoming bitter/jaded in their profession. We want to help prevent future pain/suffering as they run towards the fire now during a pandemic.” A big part of their focus has been praying for and encouraging “front-line” workers.
As they worked to flex for the needs of the community, Watermark Health has opened its first COVID testing site in the parking lot of Watermark Church. They have also been working on taking their urgent care services on the road. This week they are offering mobile testing sites at a local homeless shelter and will continue to work with other area ministries to take the services mobile.
While none of us would say that we were as prepared for this season as we would like, we don’t have to look too deeply to see how God prepared us and our organizations in ways that we are only just now appreciating. Previously I shared how lessons learned from hurricanes in New York, New Orleans, Texas and Florida helped prepare clinics to respond quickly to this disaster. Experiences overseas with Ebola and SARS have helped us understand what needs to be done now in our communities. God moved people around to be in places where they are now helping in important ways, but six months ago we did not realize why people had relocated. We questioned the change. This morning I was talking with some of the elders in our church about medical missionaries who have been called off the field for various reasons, and how many are able to plug into places like New York, or work in ER diversion programs. Those short-term needs (let’s hope they are short-term) are custom made for these unplanned short-term furloughs. Missional docs working alongside of weary ER and ICU docs are an infusion of hope. God is a great steward of resources.
We are figuring out that it is not about our own organization or our own ministries. We are part of something bigger that God is doing. I am blessed by the open-handedness that is prevalent throughout this community. Here are a few links that you may find helpful in your ministries. If you have links that you want to share, use the COMMENT section below this blog to share the link and why it was helpful for you.
He who began a good work in you/us is going to see it through. God is with you, and He does not grow weary.
In Christ’s love,
Steve
Impact on Free & Charitable Clinics
In patient care, some of your patients are more vulnerable than others. Those are the ones that concern you the most. You think about them, and are eager to know how they are doing. You see their value, and strategize about how to help them get through this.
In the same way, I have been concerned about the free and charitable clinics (FCCs) that make up 2/3 of the CCHF community. Some of those are large, well-funded organizations with permanent staff, like Crossover Ministries, Good Samaritan, Siloam or Church Health. Most of those are going to be just fine. But many FCC clinics are small health clinics with only a few paid staff, and depend on volunteers and donations to serve some of the most vulnerable people in our communities.
In patient care, some of your patients are more vulnerable than others. Those are the ones that concern you the most. You think about them, and are eager to know how they are doing. You see their value, and strategize about how to help them get through this.
In the same way, I have been concerned about the free and charitable clinics (FCCs) that make up 2/3 of the CCHF community. Some of those are large, well-funded organizations with permanent staff, like Crossover Ministries, Good Samaritan, Siloam or Church Health. Most of those are going to be just fine. But many FCC clinics are small health clinics with only a few paid staff, and depend on volunteers and donations to serve some of the most vulnerable people in our communities.
In early March I visited Katallasso Family Health Center in York, PA. (Katallasso is the Greek word for reconciliation, or for “live together”.) It is a beautiful little clinic located in an old church building in the middle of a strategic neighborhood of need. They offer medical, dental, and various specialty clinics and services for uninsured and underinsured patients. Dycelie “Didi” Rivera is the Director. If you have been to a CCHF conference in the past few years, you may have met her. Didi is a bright, outgoing ball of energy who loves Jesus and loves the people that Katallasso serves. She is good at her job, and Katallasso is a clinic you would be happy to send your mother or granddaughter to.
Clinics like Katallasso have had to make some adjustments during the COVID crisis. Kat Clinic may be small (4 full-time and 2 part-time employees); but they are a recognized and valued part of the health net in York, and participate in weekly calls with the health department, hospitals and local community health centers. Some of their volunteers are being redirected or are staying at home due to age or health issues that make them higher risk for COVID-19. There have been some financial challenges, but Katallasso remains open, focusing on non-COVID respiratory conditions, hypertensive patients, etc. They are rescheduling some of their dental and eye-care clinics, but are providing counseling and phone consults for patients who choose not to come in. They feel that their role is to be as normal as possible for their patients, and to take care of chronic health issues. Kat Clinic expects to rebound financially, and is blessed to report that patient care has not suffered over the last two months.
I also visited Heal the City Clinic in Amarillo, TX. HTC is an amazing place – a 20,000 sqft facility, with roughly 20 FTE employees, a full-scope wellness program in addition to medical, dental, behavioral health and pharmacy. Because of the role they have in their community, Chelsea Stevens, Executive Director, and her staff felt they should be part of the testing initiative for Amarillo and they started testing two weeks ago. HTC has a unique business model: They see acute care patients each Monday – anywhere from 100-200 visits in one day. Patients who need chronic care are screened and invited to become part of their “Shalom Care” program. Shalom Care patients are seen by appointment Tuesdays thru Fridays by a continuity care provider, and qualify for wellness, education and many other services.
When COVID hit, the HTC staff met to discuss how parts of this crisis could be seen as a gift, and how each person could make the most of it. They understood that it would best serve their patients to suspend some of their on-site wellness and community health activities; while encouraging those who would work from home and those most at risk to use this season to invest in their families. They contacted Shalom Care patients to check on them and to shift as much care as possible to telehealth. Roughly 90% of their Shalom Care has been by phone or video. The acute-care clinic has remained open, but patients are screened by phone before coming in. There are separate entrances and spaces for sick care. Their phone volume has increased by over 60%; but spiritual care opportunities have increased, too. Staff are praying with patients more than ever. Volunteers are making masks, helping with cleaning and supplies, and making sure the staff are cared for and encouraged. In the last few weeks they have seen a significant increase in people who have no insurance due to unemployment, and can no longer afford their prescriptions. HTC has started putting together boxes of food and basic supplies, and are giving those out to Shalom Care patients who are most in need. They plan to double that effort in the coming weeks.
Nanette Mudiam runs St. Michael’s Clinic in Anniston, AL, a small free clinic that offers an amazingly diverse scope of services. They are only open 3 days/week, but that is adequate to address the needs in a town of 20K. Their one paid nurse practitioner is normally supplemented with a number of volunteer providers. But because many of their volunteers are older, they have cut back who is allowed to volunteer. A few 65+ die-hards have been determined to come in and help during this time.
Nanette Mudiam, Executive Director
St. Michael’s Clinic
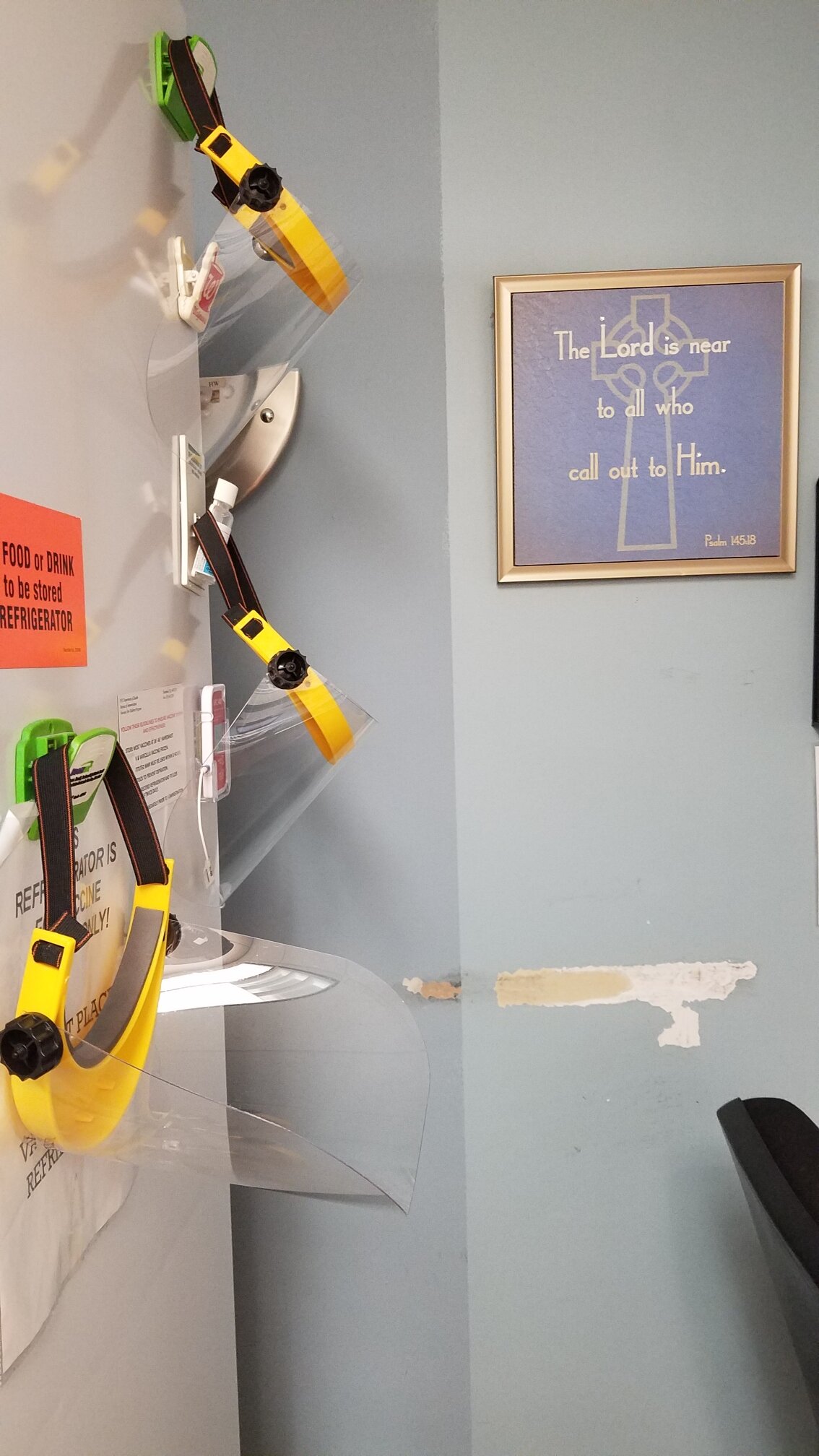
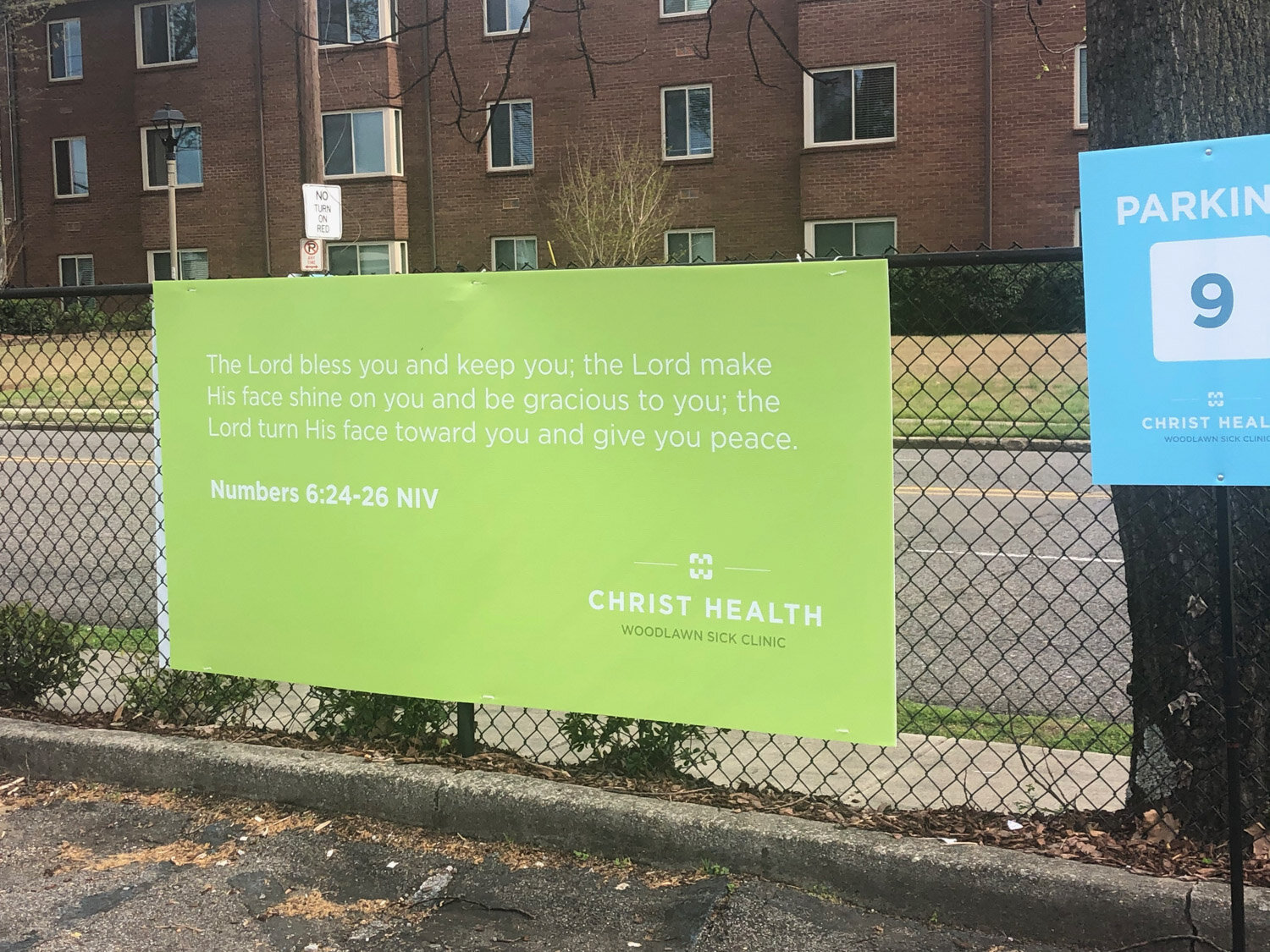
Nanette was inspired by the efforts of our friends at Christ Health in Birmingham, who helped St. Michael’s start their own COVID-Care program, providing care for non-hospitalized COVID+ patients. COVID-Care involves phone checks on patients ranging from every other day to multiple times/day, and providing whatever assistance patients and their households need in order to self-quarantine. This includes prepared food, groceries, medication delivery, tele-socializing and spiritual care. They have partnered with a local hospital to adopt patients recently diagnosed in a local housing project. All this is a stretch for their small team, but they have seen God do amazing things, using them in unexpected ways in patient’s lives. As a result, they are growing. Half of their patients last week were new to St. Michael’s.
St. Michael’s, and many other free and charitable clinics, had fundraising events scheduled between late March and early June. That is pretty typical, and they are all cancelled. Yet, God is supplying. I have heard dozens of stories of unsolicited grants and support from local foundations coming to numerous clinics. Some clinics have remained open and have extended themselves into this crisis, and they expect to come out okay financially. That seems counter-intuitive, but God provides when we are faithful to serve him.
Last Friday I spoke with Nicole Lamoureux Busby, Director of the National Association of Free and Charitable Clinics. NAFCC is an important partner with us, and Nicole is both a colleague and a friend (fellow cancer-survivor…over the years we have prayed for one another). In their network some clinics are doing amazing things, but many that feel unprepared or insecure have chosen to close for now. Of fourteen registered free clinics across Alabama, most have decided to postpone patient visits until after the crisis. The situation is similar in other states as well. I am sure there are many good reasons for some of those decisions.
A great number of the NAFCC clinics are Christian clinics, and part of the CCHF network. I am happy to report that most are doing better than I thought. God knows our frame. He uses the weak and foolish things to display his strength and confound the wisdom of those deemed wise. I plan to share more about this in a few days. Until then, is there a clinic in your area that could use some encouragement? A quick call or email to check on them would mean a lot.
In Christ’s love,
Steve
Two Very Different Experiences: Seattle
Until a few days ago it was thought that COVID-19 entered the U.S. through Seattle. Seattle was where the first diagnosed case appeared back in mid-January, and was considered the first “outbreak” city. While state and municipal governments were slow to issue stay-at-home directives, many Seattleites, especially those with high-risk family members, have been practicing isolation for a month longer than the rest of us.
There are several Christian clinics in the Puget Sound area. I spoke with CCHF friends at two of those clinics this week. Here is a summary of the experiences of Hope Central, a pediatrics clinic in the south of Seattle, and Lahai Health (formerly Puget Sound Christian Clinic), which provides primary care on the north side.
Until a few days ago it was thought that COVID-19 entered the U.S. through Seattle. Seattle was where the first diagnosed case appeared back in mid-January, and was considered the first “outbreak” city. While state and municipal governments were slow to issue stay-at-home directives, many Seattleites, especially those with high-risk family members, have been practicing isolation for a month longer than the rest of us.
There are several Christian clinics in the Puget Sound area. I spoke with CCHF friends at two of those clinics this week. Here is a summary of the experiences of Hope Central, a pediatrics clinic in the south of Seattle, and Lahai Health (formerly Puget Sound Christian Clinic), which provides primary care on the north side.
When the coronavirus began multiplying through Seattle, the north side of the city was hit hardest. One of the staff at Lahai Health tested positive, and half of the staff had to be quarantined. David Eller was relatively new as the Executive Director; but had served in medical missions overseas, and had experience in international disaster relief. He immediately began to implement changes, moving rapidly from in-person office visits to telehealth. They condensed dental services to one day/week, only for patients with emergencies. Mental health services were shifted to phone appointments. Their mobile ministry, which normally makes up a significant part of Lahai’s work, was also reduced to once weekly, and focused on patients who are experiencing homelessness.
Lahai has remained open for essential medical visits at their fixed-site clinic. Lahai (named after the place where Hagar had an encounter with God), is a charitable clinic that depends on a lot of faithful volunteers. During this time, some of their volunteer medical providers have agreed to see patients outside of the clinic. As you would expect, most of their clinical encounters are reserved for essential visits, with everything else being handled by telehealth or rescheduled for later in the year.
On the other end of town, Hope Central has had a vastly different experience. Hope Central is unique, in that they are a pediatric clinic with strong integrated behavioral health. Thirty percent of their patients are diagnosed with autism. HC’s clinic is located on the ground floor of a 6-story shelter/mission that houses women and children. Their patient population is diverse. 108 languages are spoken in their immediate community. The largest ethnic groups in their patient panel are Somali, Vietnamese and Central American.
Because coronavirus tends not to affect children in the same way it does adults, Hope Central’s providers have not dealt much with patients who have tested positive. They have been working closely with the women/children’s shelter located above them, swabbing new entries and guests who exhibit symptoms. They continue to provide basic pediatric services, working hard to keep their kids healthy, and trying to keep them on track with immunizations. But their in-office patient volume is down by 40%. They quickly pivoted to telehealth, but it has taken real effort to maintain their behaviorally challenged patients.
I spoke at length with Patricia Scott, one of the founding pediatricians at Hope Central. Her husband is an I.D. doc, and Director for Telehealth at the University of Washington; so as a family, they are in the thick of it. There are reports of new outbreaks in some of the ethnic communities in south Seattle.
While in-house patient volume is down at Hope Central, the staff have been busy trying to help families cope with isolation. With so many of their families caring for children with autism, the parents need help dealing with disrupted routines and lack of access to resources such as OT and speech therapy. HC staff created a section of their website that provides resources and tips to help families manage during prolonged times of social isolation. They initiated on-line support groups for both family members and kids, where they can socialize. They host virtual child activity meetings, where kids do things like show-and-tell. Chris Jones, pediatrician and Medical Director for Hope Central, and T.K. Brasted, Behavioral Health Director, hold live events on Facebook to help patients and their families understand this crisis better, and to provide strategies for dealing with increased anxiety and depression in the home. During these interactive sessions, parents can ask questions and have them respond in real time.
ChrisJones, M.D., Medical Director
Hope Central
While the staff at Hope Central have not had anyone test positive for the virus, everyone on staff has been stretched. “This whole thing is forcing us to become comfortable relating to one another on-line. That doesn’t seem to be a problem for our kids, but as adults, we are having to get over our resistance to ‘virtual’ encounters,” said Dr. Scott. “I think that is probably a good thing.”
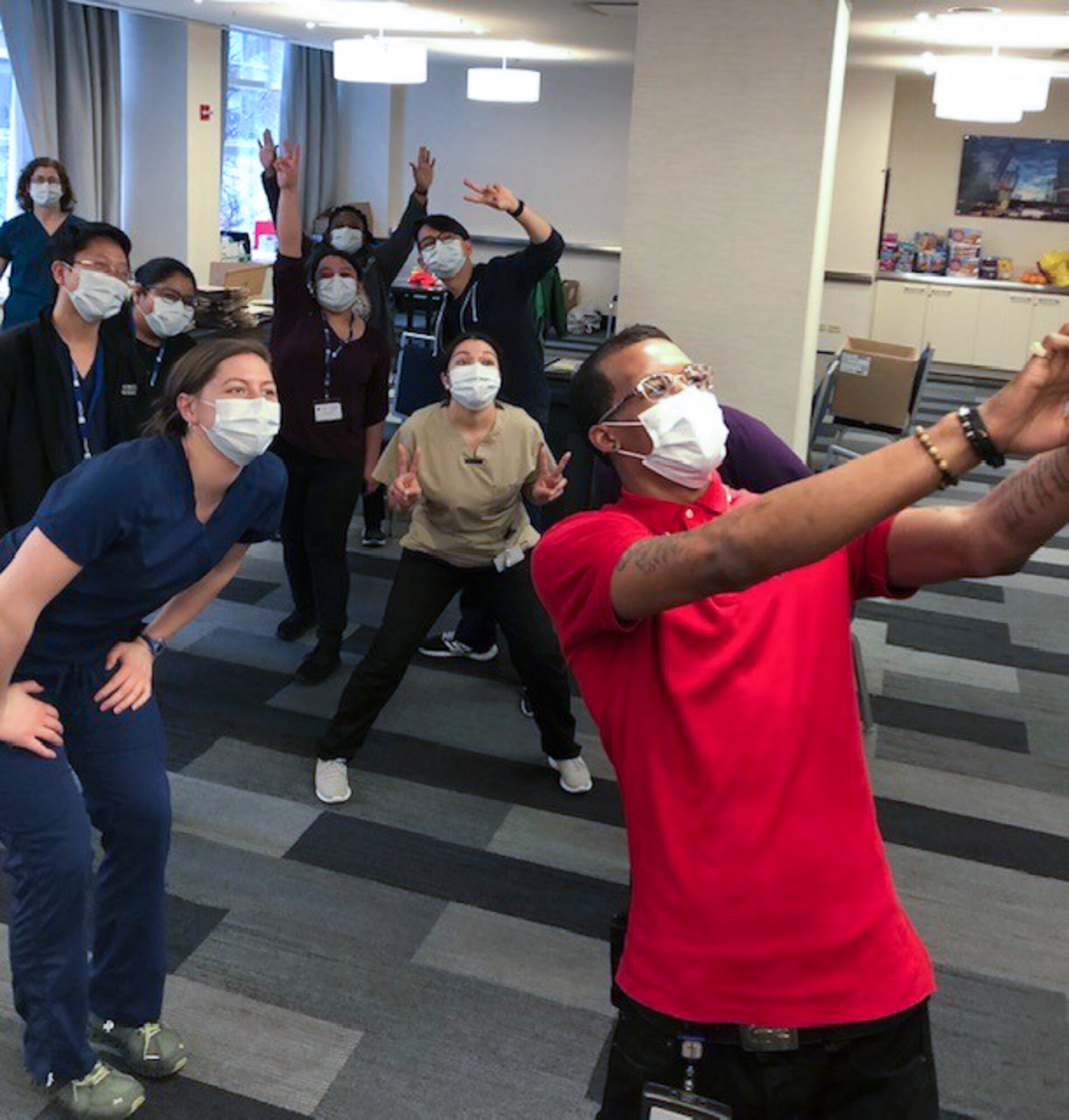
Not being together has been hard for small, tight-knit teams like Hope Central. They have had to work to maintain cohesion while so many are officing from home. Dave Kwok, executive director, has been creative about providing some lighthearted platforms for staff to connect with one another on line. And holding a daily “virtual liturgy” for staff has been helpful.
“I think this whole thing will serve as a spiritual ‘turning-point’ for not only people in the Northwest, but for people across the nation.”
David Eller, Executive Director
Lahai Health
David Eller (Lahai) shared that the spiritual climate in Seattle seems to be mixed. Seattle is not known for being a “spiritually receptive” city. During this crisis there have been many who have doubled-down on their rejection of God. But at the same time there are many who are beginning to ask sincere questions. With churches pivoting from congregational gatherings to on-line services, a number of pastors are reporting a significant uptick in non-member viewership. “I think this whole thing will serve as a spiritual ‘turning-point’ for not only people in the Northwest, but for people across the nation.” Some years ago the leadership at CCHF identified a number of “Strategic Target Areas”, geographic regions where more Christ-motivated providers and medical ministries were needed. The Pacific northwest is one of those places.
After an initial tour of Galilee, Jesus summed up what he saw: people were sick, leadership was mostly weak, missing or corrupt, entire communities were spiritually destitute, and people were isolated and oppressed. Rather than turn to his disciples and say, “Boys, this is a hard place. Let’s go somewhere else where we will be better received”, he urged his disciples that the biggest problem was not the magnitude of need, but the lack of workers. “The harvest is plentiful. The workers are few. Pray to the Lord of the harvest to send workers.”
We are grateful to David, Patricia, Chris, TK, Dave, and all those working with them for their faithfulness to extend Christ’s love in word and deed to Seattle and the northwest. Let’s pray for more to join them and us in this historic moment.
In Christ’s love,
Steve
Here are some links provided by Hope Central and Lahai that might be helpful for you or some of your patients:
www.VFAAB.org is a site for Vietnamese families with autistic children
www.hopecentralhealth.org is the main website for Hope Central. There is a section chock full of tips, resources, bulletins and videos that families will find useful.
https://lahai.org is the website for Lahai Health
CHICAGO: LAWNDALE RESPONDS
I want to give a brief report about what is happening in Chicago with LCHC during this pandemic. This will be brief, because they will figure heavily in an upcoming report where we will look at how various organizations are caring for those who are homeless. In the past 48 hours I got to speak with Drs. Bruce Rowell and Wayne Detmer, the Chief Clinical Officers at Lawndale. Here is what I learned:
Lawndale Christian Health Center (LCHC) on Chicago’s west side is unquestionably one of the most influential organizations in the Christ-centered health movement. Most of us have benefited from their successes, as well as their mistakes. We all have a little “Lawndale DNA” in our organizations. While far from perfect, Lawndale has been a progressive force, helping us all become better at living out the gospel through healthcare among those most vulnerable. The leadership has kept a culture of transparency and has been open-handed with the rest of us for over 30 years.
I want to give a brief report about what is happening in Chicago with LCHC during this pandemic. This will be brief, because they will figure heavily in an upcoming report where we will look at how various organizations are caring for those who are homeless. In the past 48 hours I got to speak with Drs. Bruce Rowell and Wayne Detmer, the Chief Clinical Officers at Lawndale. Here is what I learned:
Testing
They would like to do more, but have been hampered by lack of testing supplies. That seems to be changing. Last week they received a rapid COVID testing machine, but were still waiting for cartridges and training as of the weekend. As I write this, I received a message from Dr. Rowell that the state has guaranteed them supplies to ramp up testing, largely in response to concerns about disparate mortality rates among African Americans and people of color. The goal is to get to 100 tests/day.
LCHC started a respiratory clinic with in-car testing at their Ogden site.
Patient Volume
Normally Lawndale sees 3000-3500 patient visits per week. They are down to 2500, and that includes over 1,000 telehealth visits. LCHC has temporarily consolidated their satellite clinics into their Ogden Avenue sites where LCHC originated. They have two main sites on Ogden, 2 short blocks from one another. They are seeing pre-natal and pediatric patients at one site, while essential adult patients are seen at the other. At the adult care site, they have a special triage and sick-care entrance, and have created a respiratory clinic where patients are tested in their vehicles. They have reduced dental services to emergency only, and have closed their senior center for the time being. Other programs such as centering programs and behavioral health group sessions have been suspended. They have maintained their MAT patients, who are considered essential. Their restaurant and fitness center are also closed.
Lawndale in partnership with Chicago Department of Public Health has taken over a luxury hotel in downtown Chicago where high risk homeless patients are being housed
Staff
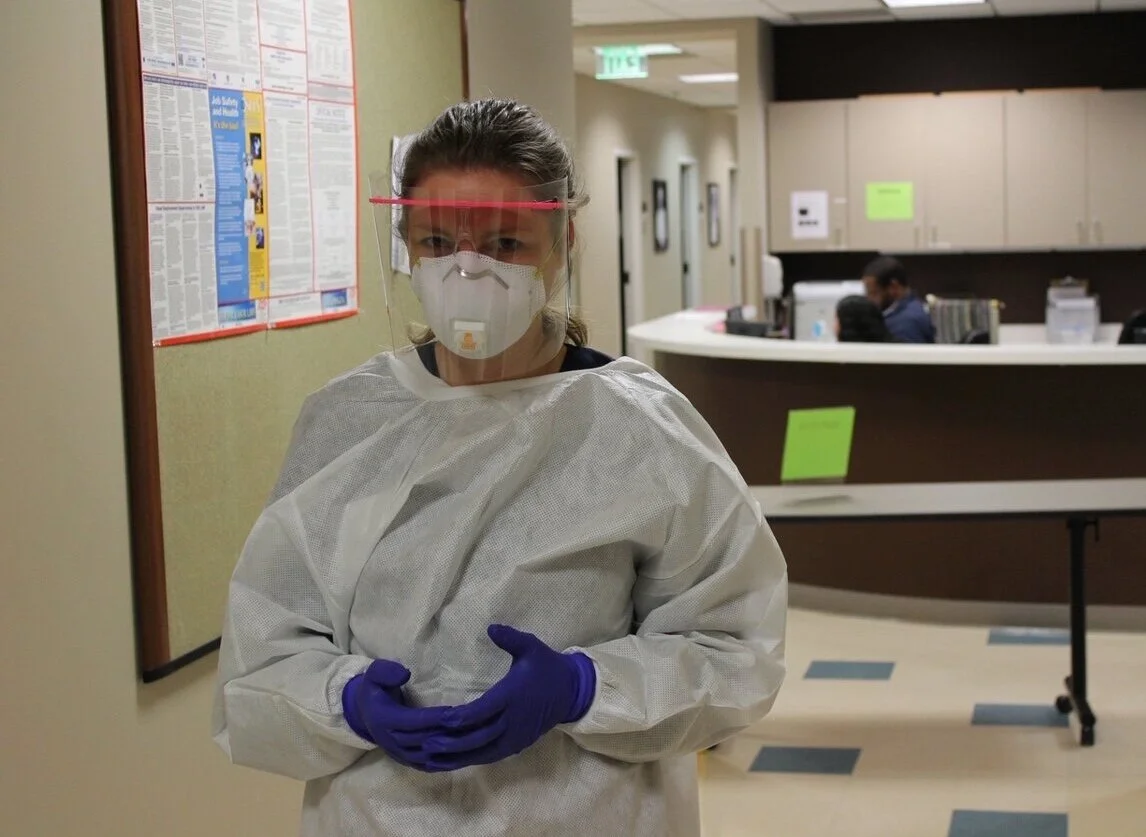
Several Lawndale staff and providers have had the virus, and a few had to be hospitalized; but thankfully they all seem to be recovering. With the consolidation of sites and services, staff are stepping into many different roles. Lawndale has always followed their patients to the hospital, LCHC providers round their own patients. Increased hospitalization volume has required a larger number of providers who are rounding LCHC patients in 3 different hospitals. Telehealth, triage and testing are being manned mostly by reassigned staff. In an effort to move high risk patients out of homeless shelters (where the positive rate is >45%), Lawndale has contracted with CDPH to take over a luxury hotel in downtown Chicago. That requires 24/7 staffing by LCHC employees and heavy rounding by providers and MAs. (More on that next week.) Many staff are putting in 14-16 hour days six days a week. People are tired, but sustaining high levels of service in spite of the relentless challenges. One doc, when asked how she was handling everything, said, “Ask me how I am doing? The answer to that question varies throughout the day.” Still, many of their providers are using any extra time they have to help in local hospitals.
charting at the hotel for their homeless patients
COVID Outlook
The hospitals where LCHC send their patients are running at about 80% capacity, so it seems like they are holding well. It is the most vulnerable populations that Bruce and Wayne are concerned about. LCHC and one other community health center currently see about 90% of the sick who use homeless shelters in the city. Behavioral health patients, MAT patients and the elderly who normally utilize Lawndale’s new Senior Center are the focus of much of the strategic thinking among the leadership.
Beyond that, everyone I spoke with at Lawndale – or any of the clinics I have interviewed – is talking about this being a marathon, not a sprint. There are concerns about “reopening the economy” too quickly and lifting isolation, and the impact that could have on both patients and staff.
—————
I realize that lifting social distancing requirements is a controversial issue. I see protests on TV with people carrying signs like “Poverty Kills Too”. And it does. We know that better than most of the folks who carry those signs. We have watched it - and screamed about it for years. Many of us work and live in neighborhoods where the life expectancy is 12-15 years lower than people who live in the next zip code – and that was before COVID. We don’t do it for money. We do it for the love of Christ and the love of those who have become our neighbors. The people we serve are suffering the most in this depression.
And yet I have not had a single provider or executive of a health clinic tell me that this pandemic is being over-played – and these are people who live and work among the very people who are being “economically crushed”. These are front-line workers and neighbors who know the names and families and communities that are being impacted by both the virus and the effects of isolation.
Forgive me if that comes across as political. I don’t mean for it to be. As I hear from you who are working on the front lines, I feel your weariness, your concerns for people who mean a lot to you, but who are a million miles away from those in power who will make decisions that could prolong or even accelerate this crisis. You are worried about your patients. But you are also worried about your co-workers and yourself. Thank you for your relentless and selfless service. I want to leave you with this. I hope you will hear it as though our Father were speaking directly to you:
“God is with you, and he will not grow tired or weary. He understands, because his understanding is unfathomable. He gives strength to the weary, and increases power for the weak. Even youths grow tired and weary, and the young sometimes stumble and fall; but those who hope in the LORD will renew their strength. They will soar on wings like eagles; they will run and not grow weary, they will walk and not fail.”
With appreciation & love,
Steve
NEW ORLEANS: ON THE DOWN SIDE OF THE CURVE
Because of the severity of the outbreak, New Orleans’ spread of coronavirus peaked on April 2, and deaths from the virus peaked five days later. New Orleans is still shut down. Isolation is still in place. But New Orleans is one of few places in America on the down side of the now famous pandemic curve.
In 2005, New Orleans took a direct hit from a category 3 hurricane. For over 100 miles both sides of I-55 were jammed with folks fleeing the storm. The city flooded. More than 70% of occupied housing was destroyed or damaged. Hospitals were incapacitated. 1,500+ people died. Over 50% of the population left for longer than 3 years, and less than half ever returned. Hurricane Katrina was a perfect storm that decimated a great city. Two months ago over a million people flocked to New Orleans. Crowds of partiers from across the country packed the French Quarter. It was Mardi Gras 2020. It was at the beginning of the COVID pandemic in America, and it was another perfect storm.
The first cases of COVID-19 in Memphis (my hometown) were from people who attended Mardi Gras. That is true of other cities as well. In New Orleans, less than fourteen days later doctors were busy treating COVID-19+ cases, and ICUs were slammed with respiratory patients. A score of New Orleanians had already died from the virus. New Orleans became one of the major outbreak cities of this pandemic. Within 3 weeks, only New York and Washington states had more cases.
Because of the severity of the outbreak, New Orleans’ spread of coronavirus peaked on April 2, and deaths from the virus peaked five days later. New Orleans is still shut down. Isolation is still in place. But New Orleans is one of few places in America on the down side of the now famous pandemic curve.
Baptist Community Health Services of New Orleans (BCHS) opened in 2013 in the Lower 9th Ward, the neighborhood hit hardest during the Katrina disaster. They now have 5 sites across New Orleans and the north shore of Lake Pontchartrain. Dr. Hannah Pounds is the CMO, and has been part of BCHS since its inception. Shawn Powers, a former missionary who lived in China for many years, is CEO. I spoke at length with Hannah and Shawn this week. I wanted to know how this crisis impacted their clinic, and was eager to hear what a clinic on the other side of the curve might share with the rest of us.
Cary Calhoun, CFO and Dr. Hannah Pounds, CMO in New Orleans’ Lower 9th Ward.
BCHS has been a Look-Alike clinic for several years, but last September their application for a new site in nearby Mandeville was approved as an FQHC. They had 120 days to get the site open, which happened on January 9. The wheels of change were already in high gear when the coronavirus threat became a reality. Shawn believes that because transformation and growth were already happening, changes to respond to COVID came easier. The comfort of status-quo was not an obstacle.
The outbreak impacted almost everyone in New Orleans. In the first few weeks, several BCHS staff members lost relatives to the virus, and one of their physicians was diagnosed COVID+. Those early days were stressful. But the staff pulled together and remained courageous throughout the crisis. The doc with the virus continued to take patient calls by phone from his home, and on one occasion God used him to help save a young man’s life.
Local church partnerships proved to be a game-changer. In mid-January BCHS’s priority turned to stocking up on supplies ahead of the virus. But suppliers were already back-ordering N95 masks and PPE. Their limited supplies quickly dwindled, and fear among staff was understandably high. During one morning devotion a team member shared the story of how God taught the Israelites to depend on him one day at a time by providing manna each morning. That morning BCHS had only 3 masks left for each site. But shortly after devotion time, a call came in from a church partner that had been part of disaster and restoration efforts after Katrina. He had found 400 N95 masks in an old storage locker and wanted to bring them by. Over the next few weeks other churches called with similar stories, and Baptist Disaster Relief was able to locate over 1000 masks for them. The staff never ran out of PPE, even during peak times.
Gloves and masks from local church partners donated to BCHS
I asked Shawn and Hannah what they would share with CCHF professionals in cities that are not at peak yet:
One practice that proved invaluable was a weekly all-staff ZOOM meeting. At first the meetings were about preparation for what was coming. But they began including a short time of ministry from local pastors, and they had a psychiatrist sit in on the meetings. Staff-care became a priority, and that made a difference.
This experience made their team stronger, and it will yours, too. They became better at rapid innovation, and policy production and implementation. They found spiritual and emotional strength in one another, and a new depth of corporate dependence on God. False assumptions and pride fell away. “We got real serious real fast about what is real important.” Events like this affirm a unifying sense of purpose.
Logistically, do the right things. Make sure your policies are in place. Figure out telemedicine as early as you can. Work your supply chain, and ask for help if you run into problems. Tighten up infection control, and be prepared to maintain those controls in the aftermath of this crisis. Get ready now for the wave of behavioral health needs that will inevitably follow this crisis. It is coming.
Make staff-care a priority. Build partnerships with local churches, and mobilize Board members and stakeholders to become care-givers to the staff. Mobilize prayer warriors. Prayer is not an option. It is the core of what causes resilience and effectiveness. Watch for effects of extended hyper-vigilance, and address those before they weaken your team.
CEO, Shawn Powers, holding bags full of N95 masks donated from a local church
Finally, know this: You are going to make it. You have been honored to be present with your neighbors in this unprecedented season, and you are a force to not only bring peace and health to them, but to direct them to God. There are already reports of great spiritual awakening across the world. You are part of something that has eternal significance.
Things are still bad in New Orleans. They may have peaked, but they are still seeing new cases daily. The city is still in lockdown. Hospital beds may be available, but the fight at the primary care level is still substantial. This is going to be a long fight; but the leadership at BCHS is committed to what they call “prayerful discovery” – seeking Christ together through prayer and counsel for ways to better address both the needs of their neighbors and the opportunities that this brings to be a more unified team with Christ at the center.
Be encouraged. Stay safe.
Happy staff with PPE, thanks to answered prayer and faithful church partners
GOOD SAM ATLANTA: NEVER WASTE A CRISIS
In a state that is famously slow to act, Breanna Lathrop was part of a team that was thinking ahead. The outbreak came, and as predicted, pockets of Atlanta have been hit pretty hard. It is nothing like NYC. But this is the South, and people don’t live on top of one another the way they do in some cities in the northeast.
Good Samaritan Health Center in Atlanta is not what most people envision when they think of a charitable clinic in a poor neighborhood. It is a beautiful facility located in the heart of one of the most distressed neighborhoods on Atlanta’s west side. They have a permanent staff, supplemented by a faithful corps of well-trained volunteers. In addition to medical services, they offer integrated behavioral health, have one of the largest dental programs in the area, an on-site urban farm and fresh market, a teaching kitchen and robust community health and education programs. It is an impressive ministry with the gospel at the core of all they do. And it has been a flagship clinic in the CCHF/Christ-centered health movement for many years.
Early last month I visited Good Sam and met with Breanna Lathrop, DNP, MPH, who serves as Good Sam’s COO. At that time, many of us were not convinced that COVID-19 was going to be the big deal it has become. People were still filling arenas for concerts and to watch NBA games. We were still planning to hold the CCHF conference; and fans of Duke, Gonzaga, Kansas and Kentucky were looking forward to March Madness. Most of the CCHF clinics were watching the coronavirus, but few were making any solid plans or strategies to deal with it.
Founded by Dr. Bill Warren, Good Samaritan Health Center, Atlanta, served over 37,000 patient visits in 2018, which makes it one of the largest charitable clinics in America.
For weeks however, Breanna had been part of a region-wide COVID task force that was raising issues about what a outbreak would look like in Georgia. They had been advising city officials and health systems to get ready. In a state that is famously slow to act, Breanna was part of a team that was thinking ahead. The outbreak came, and as predicted, pockets of Atlanta have been hit pretty hard. It is nothing like NYC. But this is the South, and people don’t live on top of one another the way they do in some cities in the northeast.
Breanna Lathrop, DNP, MPH is COO for Good Sam Atlanta
Fulton County, where Good Sam is located, has the highest incidence of the virus in the state. As of today, Georgia is only reporting 13,315 confirmed cases of COVID-19. But testing has been slow and spotty across the state. The real numbers are suspected to be much higher; and Atlanta is not expected to peak until May 1. Most testing is done at drive-thru testing stations run by Georgia’s Department of Public Health, and are by referral only. Good Sam has had to refer out for testing, but is treating and managing COVID+ patients, often before the patient can get an appointment to be tested. Good Sam plans to start testing as soon as blood tests become available – possibly this week.
Patient care at Good Sam is similar to what other good primary care clinics are doing – screening by phone, outdoor triage, separate entrances and isolated areas for patients with fever or other indications for the virus. Forward thinking allowed them to stock up on supplies, so staff have PPE. The waiting room is now in the parking lot. Their patient volume is down like everyone else’s, and they are doing a lot through telehealth. Many of their ancillary services have been put on hold. They are working to keep people out of the ER.
But in addition to addressing the immediate needs of their patients, Breanna and the team at Good Sam have focused on two other issues.
Social distancing: Good Sam has moved the waiting room to the parking lot. Many of their patients take a bus or walk to the clinic. For them, the waiting room looks like this.
They recognized early that charitable clinics across Georgia, especially many of the smaller ones, were poorly prepared for this crisis and had started making plans way too late. A number of clinics simply shut their doors, not knowing what to do. Good Sam realized that they could be a resource for smaller charitable clinics in the area, who are needed to continue to manage their patients’ chronic health issues now more than ever.
So Breanna and Veronica Squires, Good Sam’s Chief Administrative Officer, made their protocols, manuals and resources, along with resources from the Coronavirus Support Network, available to charitable clinics across Georgia. Working with the Georgia Charitable Clinic Network, they are helping clinics adopt best practices and making sure they have the support they need to fill gaps in a state that has a lot of gaps to fill. I recently spoke with Breanna and Veronica. “We don’t expect clinics without the staff and resources like we have at Good Sam to do what we do. We tell them that ‘What you do well is what you should do now’. They have a part to play, and we all have to stay in the game.” Breanna started a blog, which has helped a lot of providers and clinics understand what to do. (There are links to these resources at the end of this article.)
One of the challenges Good Sam faces in the African-American community in west Atlanta is overcoming well-earned mistrust toward the medical community. “Inequities are magnified in a pandemic. Social distancing is a privilege that the poor cannot afford. They lack the resources, space and logistics to purchase and store food for a prolonged isolation. And people don’t trust the government or the medical institution. In our community many still remember the Tuskegee experiments on African American men. We are seeing the generational and systemic brokenness that has led to disparities and barriers to care. They can’t be denied or ignored anymore.”
The COVID pandemic highlights systemic disparity on many levels. Jerome Adams, U.S. Surgeon General recently stated, "We do not think people of color are biologically or genetically predisposed to get COVID-19”. Rather they are more susceptible because they “have a higher incidence of the very diseases that put you at risk for severe complications of coronavirus.” Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said last week that African Americans "are suffering disproportionately," adding that, "When they do get infected, their underlying medical conditions wind them up in the ICU." Paul Keckley, in his weekly blog, observes “The CDC findings are the latest evidence that social determinants of health, not genetics, explain why people of color in our society are less healthy, die younger, and access the health system less frequently even when it’s necessary.”
Between 1932 and 1972 the United States Public Health Services conducted a study on 600 impoverished black males to observe the effects of untreated syphilis. The men in the study were only told they were receiving free health care from the Federal government of the United States, and that they were being treated for “bad blood”. These wounds are still fresh among many in the African American community, who believe that people of color have always served as the “lab rats” for the institution of medicine.
Breanna and Veronica are using this pandemic as a megaphone to highlight these issues. They co-authored book that is an excellent primer for addressing social determinants of health called, “How Neighborhoods Make Us Sick: Restoring Health and Wellness to Our Communities” (IVP Press).
I appreciate Breanna, Veronica, and CEO, Dr. Bill Warren, for thinking ahead, and for thinking beyond the clinical environment of Good Sam. They used their position, relationships and experience to influence those in power, and to assist other Christ-centered and charitable ministries.
A friend recently reminded me of a Winston Churchill quote, “Never waste a good crisis”. I wouldn’t call this crisis good, but let’s not waste it anyway. This is a time when, for once, we are not invisible. The spotlight is on health professionals for serving courageously in the fight against an invisible enemy. Health workers are center stage. (Rio de Janeiro’s iconic Christ the Redeemer statue is even lit up as a doctor to honor health workers. A nice gesture, but don’t let it go to your head!) With true humility, let’s use this opportunity to co-own the brokenness in our healthcare system, to witness to the systemic dysfunction that has attributed to the vulnerability of those we serve, and to be a platform, a voice and an example for reconciliation to the church, to medicine, to the powers that be, and to the communities we love.
Stay safe. Stay faithful.
Links:
https://goodsamatlanta.org/COVID-19/
https://coronavirusnetwork.org
https://www.ivpress.com/how-neighborhoods-make-us-sick
PASSOVER GOES VIRAL
I went for a short walk on Tuesday, and a lamb was walking down the middle of the street. Yep, a lamb – a little baby one. I live in Memphis. We don’t have sheep here. Some of my neighbors keep chickens, but no lambs. This one had no collar (do you put collars on lambs?), and no markings. Because there are many stray dogs in my neighborhood, I “shepherded” the lamb to the nearby schoolyard and called animal services. I “rescued” a lamb two days before Passover. It must be a sign.
I went for a short walk Tuesday, and a lamb was walking down the middle of the street. Yep, a lamb – a little baby one. I live in Memphis. We don’t have sheep here. Some of my neighbors keep chickens, but no lambs. This one had no collar (do you put collars on lambs?), and no markings. Because there are lots of stray dogs in my neighborhood, I “shepherded” the lamb to the nearby schoolyard and called animal services. They came and got it and took it to safety.
I rescued a lamb two days before Passover. It must be a sign.
My granddaughter and the lady from animal services.
(I took the picture at a safe distance more than 6’ away)
Victoria and I are part of a group of house-churches, small groups of disciples who meet in homes as we try to walk out life in Christ together. For the past decade, our house-churches have celebrated Seder. I am not much on religious tradition, but we really enjoy Seder. It is a party with people we love. We enjoy a long dinner with good food and lots of wine, and we remember traditions that help us contemplate the significance of the death and resurrection of Jesus. We read a long liturgy (12 pages single-spaced) that tries to be faithful to the Jewish tradition, and still highlight how Passover is fulfilled in Christ. It’s a joyful feast with lots of laughing as we get hung up on Hebrew words that are unfamiliar to us. (None of us come from a Jewish tradition. I am sure we butcher it badly, but we have fun.) We always end with a fire in the fire pit, where we burn what is left of the lamb (a Biblical requirement), and finish off the wine (not a Biblical requirement).
But no Seder feasts this year. At least not together.
I have always looked at Passover as a remembrance. But that was not the way it was at the first Passover. Bits of the feast were intended to remind them of the hardship and brokenness they experienced in Egypt, hardship that most of them experienced earlier that day. It didn’t take much looking back. But a lot of the Passover instruction was mystery, and most of it was about the participants getting ready for something.
One of our house churches a few years ago. Some have moved to the mission field. Some have gone to be with the Lord.
Put yourself in their sandals. An order went out that everyone was to go home, isolate themselves and shut their doors. They were to thoroughly clean their homes. If they were to go outside, they might die. If they stayed inside, they would live. Sound familiar?
The first Passover meal was not a party. It was not to be shared in a large group. Each family had their own meal. They each had to butcher their own lamb, had to make their own preparations – preparations to move. It was a time of examination - What is important? What can we leave behind? God said he is coming to deliver us, but what will that look like? They were to eat with staff in hand, with their traveling clothes on. The unleavened bread thing was about being ready, eating in haste. It was a far cry from our lengthy parties (which I still love and intend to enjoy in the near future). The first Passover was probably taken in an environment of fear and uncertainty. And faith.
All that to say – and I am asking an honest question here – could this be a prophetic moment for us? Could this Passover/Easter be different than others? Could this season be one that will forever change our lives, that will bring us into new freedom and that gives us an opportunity to experience God and the fulfillment of his promise on a scale like never before?
Why not!
We are having a worldwide “Passover”. This is an historic moment. The pandemic has forced everyone to isolate, to shut ourselves in our homes, not unlike Moses’ instructions to the Israelites. And what we are doing behind our closed doors will determine the future.
Perhaps this should be a time for self-examination, cleaning house, and getting ready to follow God. This weekend, as we reflect, maybe we should look forward as much as we focus on remembering. Maybe we should remind ourselves of the brokenness we see around us, and call broken what is broken. Maybe we should eat with staff in hand and sandals tied, with our traveling clothes on. Maybe this is a time to cry out to God in a deeper way than ever before. And maybe he will deliver us on a scale like never before.
Are you a little afraid? I am; but it’s not the virus that has me nervous. I am filled with anticipation. God may lead us somewhere very different…different culturally, different in terms of priorities, into new depths of understanding of his ways and experiencing him. I have learned from 40+ years of following Jesus that every decision to follow is a decision to leave something dear. So, yes, I am afraid. Maybe we should be.
Maybe the church will look differently. Maybe our nation will change. I don’t know. I know that I have become far too comfortable with a status quo that is broken – I am referring as much to my own familiar, comfortable brokenness as I am to brokenness in this world. Maybe this will be the greatest Great Awakening in history…a worldwide Great Awakening! I have very little to do with that happening, but I can certainly prepare for a great awakening for me. How about you?
The first Great Awakening saw people turn to Christ in unprecedented numbers and changed paradigms for government and society (though not enough). John Wesley, Jonathan Edwards and George Whitfield were key figures in the Awakening, all men in their 20s and early 30s.
A few weeks before Christmas, one man in China coughed, and the world fell apart. Economies crumbled. Science and medicine proved impotent. Politicians failed us. Institutions of academia ground to a halt. Commerce collapsed. The powerful military proved to be as vulnerable as the rest of us. That is not to say that there are not heroic individuals who have risen to this challenge. I know a lot of those heroes, and I am grateful for them. But the Institutions that we look to for security have proven to be sandy foundations. Coronavirus leveled us, rich and poor, red and blue, first world and third world, east and west. We are all in the same boat.
And yet we are surviving. It turns out that while everything is being shaken, the unshakable kingdom of God still holds strong. We are recognizing that our true leaders are servants, and we are grateful for them. Those who were invisible a month ago are our heroes now. I stand on my porch every Wednesday morning to thank the sanitation workers who take away our trash. We applaud those who work in hospitals and testing sites, and those who stock our grocery’s shelves.
Humility, obedience, simplicity, family, faith, prayer, and compassion are proving to be a foundation that doesn’t fail us. Righteousness and justice move us. We call out hoarders and profiteers, and share what little we have with those who are in need. Unemployment is through the roof, but so is generosity. Doing what Christ taught in his sermon on the mount and by the testimony of his life is the rock that keeps our lives from collapsing. To the degree we cling to that rock, we will be ok.
Normally at this time of year I end with “He is risen!”. He has risen indeed, and not for naught. I am unusually expectant. Aren’t you?
Happy Easter. Get Ready!
PS - (Added Friday morning) At the last minute we decided to pull off Seder with members of our house-church via ZOOM. Here is a pic of what that looked like. Not the same as being together, but we still managed the liturgy, 4 glasses of wine, some much-needed fellowship, and thanksgiving to God for His amazing love, demonstrated by sending Jesus to us. HAPPY EASTER!
UNIQUE ISSUES IN LOS ANGELES
Los Angeles was the site of the first person in America to die of COVID-19. Yesterday (April 6), there were 420 new cases of coronavirus in Los Angeles County. Roughly half of the +15K confirmed cases in California are in the Los Angeles area. Compared to what is happening in New York, that may not sound so bad. But Los Angeles has its own unique issues, and our friends at Los Angeles Christian Health Center is working hard to get ready for the worst.
Shannon Fernando, Chief Innovations Officer and Carolina Maradiaga-Esguerra MA Supervisor, serve a unique population at Los Angeles Christian Health Center
Los Angeles was the site of the first person in the United States to die from COVID-19. Yesterday (April 6), there were 420 new cases in Los Angeles County. Roughly half of the +15K confirmed cases in California are in the Los Angeles area. Compared to what is happening in New York, that may not sound so bad. But Los Angeles has its own unique issues, and our friends at Los Angeles Christian Health Center is working hard to get ready.
Between 7,000 and 10,000 people live on Skid Row, an area famous for one of the largest populations of homeless people in America. Skid Row got its name in the 1930s from being a place where people were living “on the skids” – at the bottom of society, no jobs, no money, no place. It is home to a number of shelters and rehab programs. The movie, The Soloist, a true story about a talented cellist who became homeless when he developed mental health issues (Jamie Foxx and Robert Downey, JR – a good flick recommendation while you are isolating) was filmed right outside of Los Angeles Christian Health Center. LACHC has been located in Skid Row, caring for a vulnerable, chronically homeless population for 25 years. Only one confirmed COVID+ patient has been diagnosed on Skid Row, and that person was not homeless. But the providers at LACHC know their neighbors, and they know that when COVID hits, it is going to be bad.
For the past two weeks LACHC has had an outdoor triage station at their two main locations, and have been offering free testing. But they have met resistance. A conspiracy theory runs rampant in the homeless community that COVID-19 is a hoax, fabricated by the government to get rid of those who are homeless. At LACHC’s Boyle Heights site, 1.5 miles to the east, patients resist testing because many are undocumented, and fear that testing will put them “in the system”. In their first few days of testing, not one person came. After 10 days, they had only tested 40 people.
Like everywhere else, patient volume has dropped off in their clinics. For unhoused patients, this is a particularly bad problem. Many have mental health issues in addition to everything else. Telehealth may be an answer for a lot of clinics, but homeless people rarely have phones. Those who do don’t usually keep them for more than a few weeks.
Social distancing, isolation and quarantine are huge problems for the homeless. Most have no secure housing and no way to store food. The typically crowded shelters are making changes to try to enforce social distancing; but lower density in the shelters translates into more people living on the streets.
LA County has been proactive at addressing the quarantine issue. In an effort to create a COVID quarantine zone, they placed 112 RVs on Dockweiler Beach, about 40 minutes from downtown LA. They want to use the RVs to quarantine COVID+ homeless patients who do not require hospitalization. But many fear that if they go there, they may not be able to get back to Skid Row, where they know people and can find familiar resources to survive. In other areas where unhoused people present with fevers, they are given tents and told to stay in them for 2 weeks. There is hope that the city might place 10-15 trailers in front of LACHC’s Skid Row site to help with the quarantine problem.
LA County has placed 112 RV’s at Dockweiler Beach, 40 minutes from downtown, to create a quarantine zone.
Meanwhile, the staff at LACHC courageously put themselves at risk with this largely untested, challenging population.
They have teams who rotate at the Dockweiler Beach quarantine areas, checking on patients and trying to keep them out of the hospitals
Their four “Street Medicine Teams” visit those who are experiencing homelessness where they live, identifying those who are sick to get them tested and isolated, and trying to bridge the cultural resistance to testing and social distancing
LACHC mental health teams stay busy trying to maintain the health of their most vulnerable patients
LACHC staff continue to offer street testing and triage at their two main sites
Most of the leaders and providers are working 12-14 hour days. What keeps them going are times of prayer and devotion, which have become indispensable. LACHC has a robust mental and behavioral health team, who are also caring for the care-givers and staff.
Dr. Katy White, CMO,
Los Angeles Christian Health Center
Dr. Katy White is the CMO and sees patients at the Pico Aliso (Boyle Heights) site. In spite of all of the challenges they are facing, she sees God doing some amazing things. “I’ve been blown away by the courage and fearlessness of our staff. I see servanthood like never before from our providers, and from the rest of the staff, too. We are seeing different sets of gifts rising to the top, and leaders emerging during this crisis. We are weeks away from any kind of peak. We are still very much preparing for what is to come. And it is tough. But I see God doing awesome things in our staff and team.”
Special thanks to Bettina Lewis, COO, and Katy White, CMO, Los Angeles Christian Health Center
UPDATE FROM NYC
Because of the volume of interest in the stories we have shared, we felt it would be helpful to give an update from one of the leaders of Beacon Christian Health Center (Staten Island). I received this from Dr. Janet Kim at Beacon last night:
This is what is in fashion in NYC!
Beacon providers ready for testing
Because of the volume of interest in the stories we have shared, we felt it would be helpful to give an update from one of the leaders of Beacon Christian Community Health Center (Staten Island). I received this from Dr. Janet Kim at Beacon last night:
I've been meaning to write this message to you to share with the rest of the CCHF family. We are nowhere near peaking in Staten Island and I am sure it is the same in the rest of the city. I want to share the following with our CCHF network. Here is my message to share:
Please learn from what NYC has experienced in March. The best thing that you can do now is TEST, TEST, TEST. In early March, we had no rapid test kits. All we had was 55 test kits. Short on PPE, we only tested 4 per week - and only those according to CDC priority groups (symptomatic, >65 years or with chronic diseases). God blessed us with additional PPE and now this week alone, we have been testing 5-6 PER day. It used to take 4 days to get results. Now it is 6. When we test, we are testing those who are symptomatic. We are not testing anyone who simply say they were exposed but have no symptoms.
Beacon clothesline: PPE washed and hanging to dry for next use
Next week we expect to receive 500 test kits for rapid testing that will give us results in 15 minutes, and which do not require full PPE because it is a blood test that requires one drop. This is a game changer for us. You see, 3 weeks ago, NYC Dept of Health mandated that all outpatient testing must stop in order to conserve PPE. However, we kept going with our 4 per week. Now we are doing up to 5-6 per day. And next week, we hope to start our rapid test kits.
The other thing to share is that COVID19 is the “Great Mimicker”. I used to follow the chart that shows the difference between flu, corona, and allergies. The more I see COVID+ patients, the more I realize that chart is unreliable to know how to diagnosis without a test.
Fever is the major sign that should raise a flag to test for COVID. However, there are some patients that only present with GI symptoms (diarrhea, nausea, and vomiting) and with loss of taste and/or smell. These symptoms usually last a few days, and the sensation deficit returns in 1 week. Those with respiratory symptoms start with low fever that will last for up to 1 week. Around that time you need to watch for cough and mild respiratory symptoms. That is when shortness of breath can kick in.
NYC stopped doing outpatient testing 2-3 weeks ago, and told the public to stay home with mild respiratory symptoms without any antibiotic intervention. These are the patients that are crashing and have to be placed on ventilators. Mortality greatly increases when you end up on a ventilator. Our goal should be that patients do not need ventilators because we manage their mild respiratory symptoms early.
For this reason, we are aggressively starting people on antibiotics even with just a cough (with other symptoms, as well). I am not one to be liberal with antibiotics; but for this season, I am very liberal in writing scripts. In NY, it is almost IMPOSSIBLE to get hydroxychloroquine outside of the hospital because of our Governor's order to mandate HC for treatment in the hospitals. Instead we opted with an antibiotic protocol that we had forwarded to us from Spain. Along with this, we call our patients daily to check up on them for at least the first 5 days. When we call, we also screen for social determinants of health and for spiritual needs.
Now that rapid tests are coming out, test as many symptomatic patients as you can. Do not assume that it can be flu or allergies. The best thing to do is to test and to isolate those who test positive. Reinforce the importance of strict isolation with your patients. Once you find positives, they need to strictly quarantine until at least 3 days without fever AND 7 days without any symptoms. We are finding many of our non-English patients come from crowded, multigenerational homes. When we do telemed visits with them, most are not wearing masks or following strict isolation rules. This is so important.
Primary care and community health education has been understated in the media. There needs to be coordination between primary care and the hospitals. Even if you think your role is small, please do not underestimate your role as a FQHC/free clinic/private practice/parish practice, etc. One of my close friends was the team lead for a recent WHO team to Wuhan. When I was struggling to know what to do in our clinic's response, he told me: "As a Christian, you need to do the right thing. Your patients in your community...they trust you. They are coming to you because they know you can help them." This has helped me shape our approach and response.
We pray that none of you will experience what we are seeing here. Our hope and anchor is knowing that Psalm 91 and 23 are true and reliable. We are existentially seeing God's faithfulness and protection. If you are in an area that is not a hot spot, you have time now to prepare. If you are in a hot spot, it's still not too late to act.
Drs. Janet and David Kim
My husband has been saying: “Firefighters run to the fire not away from it; our job as health care workers and safety net providers is to serve our patients and help them to stay healthy or to help them get better.” We cannot and should not shy away from COVID19. We do not have to be like sitting ducks waiting for the inevitable. There is a way to respond that will give hope to all.
Janet Kim, MD, MPH, FAAP, MA (Bioethics)
Chief Medical Officer
Beacon Christian Community Health Center
Janet has offered to share resource contact information with anyone who needs them. You can find their contact information at https://www.beaconcchc.com
On deck: stories about Southern California, Seattle, New Orleans and Atlanta. We will be exploring how clinics are protecting and caring for those who are experiencing homelessness, and how they are serving refugee populations. I am deeply concerned about how this crisis is impacting CCHF charitable clinics that are heavily dependent on volunteers. We will be checking in on them.
Feel free to share this with your co-workers and with peers at other organizations. Stay safe. Be wise. Make the most of this time.
In Christ’s love,
Steve Noblett, and the CCHF team
Leading in a Crisis
A month ago, when we were all still questioning how big a deal the coronavirus was going to be, Dr. Myron Glick met with his team at Jericho Road CHC (Buffalo, NY) to address how they would go about making decisions when the time came. They defined their guiding goals, the role would they play, what their priorities needed to be. I am sharing his email…
Dr. Myron Glick, CEO, Jericho Road Community Health
Photo by Derek Gee, Buffalo News
A month ago, when we were all still questioning how big a deal the coronavirus was going to be, Dr. Myron Glick met with his team at Jericho Road CHC (Buffalo, NY) to address how they would go about making decisions when the time came. They defined their guiding goals, the role would they play, what their priorities needed to be. I am sharing his email to me, only slightly modified, not because I think we should all do what Jericho Road is doing, but because I found it to be a helpful template for guiding leadership and decision making. At the end I will give a short update on how Jericho Road is doing.
Steve, this is what we are doing at JR during this crisis. It is an evolving situation. It is going to get worse.
Through this all I have 3 Main Goals:
Stay open as a primary health care center for the vulnerable population we serve and also be able to continue to do our hospital work and deliver babies
Protect our staff
Stay financially solvent
Our Plan:
Aggressive screening of every patient and staff before they enter our health centers or program buildings. We started this last week.
Any person with fever and/or respiratory symptoms, even if they have no travel history, are being treated in separate areas of our buildings with providers wearing masks and gowns. We also are isolating folks with high risk travel history.
We are starting to give each of our providers the capacity to do Telehealth visits for any of their elderly patients or at-risk patients on their schedules instead of making them come in.
We have been pushing the leaders of the hospitals where we deliver babies and have our adult service to be more aggressive in getting ready for this.
We have been aggressive with screening all the people who stay in our homeless shelter for asylum seekers every morning for symptoms. (About 100 people per night) because we know that could be a big challenge if we get a positive case there.
In addition, we are trying to be proactive with regards to our finances, given that it feels like we are entering a challenging time with decreased productivity etc.
We are temporarily closing some of our community based non-medical programs and some of the staff that work in these programs are either reassigned or laid off.
We have instituted a freeze on all new hires even for positions where we have lost a person, except for new medical providers.
Finally, we have halted all international travel and interstate travel for our entire staff. I have had to cancel three JR global team trips that were planned for this spring.
This is the biggest challenge we have faced at Jericho Road since we started 23 years ago. Definitely praying for wisdom, courage and protection. Our team would be happy to help others if they have questions about how to get ready themselves. Would also be happy to learn from what others are doing.
Myron
That was a month ago. Some of those “plans” have been adjusted.
Being hit with a crisis that virtually everyone has underestimated presents special challenges for leaders. For those of us you are not in leadership positions, we need to show some grace for our leaders. We need to pray for them, stay calm, and expect lots of changes. For those of us who are leaders, we strive to be responsive, but not reactionary. Defining our goals, roles, and priorities is an important step. In practice, that is not always our first step; but it is never too late to take a breath and make sure we are working within those parameters.
In addition to 3 sites, a refugee drop-in center, and a shelter for asylum seekers, Jericho Road starts and supports clinics in Sierra Leon and two other countries overseas.
The verse in Philippians that says “I can do all things through Him who gives me strength” doesn’t say “I can do everything…”. We can do what we are supposed to do. He gives us the strength for that. And if we ask and listen, He will give us the wisdom we need, too.
I spoke with Dr. Glick this weekend. Here is a quick update:
They closed one of their sites and consolidated services into their two largest, most secure sites.
Patient volume is off like everyone else’s. 50% of their visits are tele-health visits now.
Thirteen of their staff have tested positive for COVID-19. None were symptomatic at work, and it is likely they were infected elsewhere. All have mild symptoms.
Given the number of staff and the fact that many are refugees living in multi-generational homes, they expect more over the next few weeks. Western New York is far from peaking.
This has been a highly emotional time for staff: Co-workers are sick…temporarily closing a site where the staff are particularly invested in the community…dealing with COVID+ guests seeking asylum shelter…concerns for overseas clinics and workers who are poorly resourced when it hits their regions.
Several Board members have taken over care for their COVID+ staff, calling them daily, praying for them, making sure they have food, etc.
Local churches have mobilized members to sew masks and gowns for the staff, covering each with prayers for those who will wear them.
Myron also shared that this crisis, the most difficult that their clinic has encountered, is making them stronger. They are learning how to function efficiently and lean. Their managers are developing strong leadership and sharp decision-making skills. He is proud of a staff that is emotionally invested in one another, in their communities, and in their global work. While painful, there are many things to be thankful for.
Stay safe. We are praying for you. We are all in the places we are for such a time as this.
In Christ’s love,
Steve Noblett
Working to Stay Ahead of the Curve
Ten days ago, Alabama reported that they had zero confirmed cases of COVID-19. When pressed, it turns out that Alabama had done almost no testing. This inspired Dr. Robert Record, CEO for Christ Health Center (CHC) in Birmingham, to take the initiative to find testing for their patients. Last week Christ Health Center, in partnership with Church of the Highlands and a local testing lab, opened a drive through testing center. In 5 days they performed 2267 tests. They have received just over 2200 results back, and had 73 people test positive for COVID-19.
Ten days ago, Alabama reported that they had zero confirmed cases of COVID-19. When pressed, it turns out that Alabama had done almost no testing. This inspired Dr. Robert Record, CEO for Christ Health Center (CHC) in Birmingham, to take the initiative to find testing for their patients. Last week Christ Health Center, in partnership with Church of the Highlands and a local testing lab, opened a drive through testing center. In 5 days they performed 2267 tests. They have received just over 2200 results back, and had 73 people test positive for COVID-19.
Robert had a contact with the founder of a private testing lab who had been trying to implement testing, but was overwhelmed. He visited his friend one Saturday, and listened to him talk about the challenges that the lab was not prepared to meet. Robert proposed that Christ Health set up and do the tests, while allowing the lab to process the respiratory panels, which is what they were good at doing. Robert and his team met with the leaders of Church of the Highlands, a mega church where Dr. Record and a number of the staff attend, and a church that has been a close partner throughout the development of CHC. In only a few days they designed a drive through testing model that is a national model of efficiency, trained staff and a small army of volunteers, published a video, and implemented the largest testing center in the state, and one of the largest in the country.
If all of this sounds like something slapped together, watch this 9 minute video. It is impressive.
Almost immediately, Dr. Record and his team began thinking about how those who would test positive would receive care. As he was praying early one morning, he got a picture in his head of what they should do. They trained UAB (University of Alabama at Birmingham), which is the largest hospital system and employer in the state, how to do the testing. Christ Health has now turned their drive-thru testing over to them. Simultaneously, they constructed four “bubble rooms” in the building next to their clinic to care for sick patients. These plywood and plexiglass exam rooms allow the doctor to interact with the patient, but from the safety of being on the other side of the glass. They instituted a text-to-access system for positive patients. They started seeing COVID+ patients today (3/25) to work out any bugs in their system.
Christ Health’s medical director, Dr. Cleon Rogers, is overseeing “COVID-Care” for the 73 positive cases that they tested who are not hospitalized, plus is taking non-UAB patients who test positive through UAB’s efforts.
They provide safe, best-practice care for all of their COVID positive patients primarily through telehealth calls and visits.
They do frequent telehealth check-ins – daily for high severity patients, and every other day for low severity patients.
They created an internal “off label” use protocol in conjunction with academic infectious disease and cardiology to offer hydroxychloroquine/azithromycin treatment with informed consent for their high risk COVID positive patients.
They provide wholistic care for their COVID positive patients, including, where needed, food and prescription delivery, and spiritual care. They do this in collaboration with their church partners.
While they are only 6 days into this COVID-Care program, so far none of their patients have required hospitalization. “Being able to keep 73 people at home is huge! And we are not just providing for those 73. Each one of them live with family members, and we are providing this care to everyone in the house during their quarantine”, said Dr. Rogers. If this model proves fruitful, Dr. Rogers will be sharing this resource with the medical community soon via a paper and video. We post those links on the CCHF website when they become available.
How has this impacted their other primary care efforts? Christ Health does a fairly large volume of behavioral health work, and those visits seem unphased so far. In terms of medical visits, they continue to see their mental health and higher risk patients, but in-office volume is down by about 50%. The rest of their work is going forward through tele-health.
You might wonder how all of their efforts are funded. Christ Health is an FQHC, and some of the visits and testing is billable. But uninsured patients are tested for free, and they opted to not collect any copays for their insured patients. They raised no money for any of this. “We were ‘action first’, and then trust God for resources. We don’t want to be fiscally irresponsible, but God has met both us and our patients.” said Dr. Record. “We saw what was and wasn’t happening, and we entered into the pain of our patients and my friend at the lab. We knew we had to do something, and show that it could be done quickly.” Private funders, having heard about their work, have sent unrequested donations after the fact. That has helped. The state health department has provided little or no help. The government mechanism was simply moving too slow. To date, 80% of COVID-19 testing statewide is being done by the private lab that partners with Christ Health; and 25% of all COVID positive patients in Alabama are how receiving care through Christ Health.
Dr. Record, Dr. Rogers and their team are well ahead of most of us in the CCHF community, and wide open to share processes and procedures with other CCHF clinics. Dr. Record: “If you are going to share one thing with the other clinics, tell them that we need to turn our attentions, energy and resources from testing to treatment. That is where we need to be leading at this point in the curve.” Dr. Rogers: “We should not underestimate the impact of spiritual care for these patients. God has opened doors for me to provide meaningful spiritual ministry to my patients every day.”
A Beacon in NYC
According to the New York Times, New York state has roughly 5% of coronavirus cases worldwide, and New York City has over 25% of all COVID-19 patients in the US. As of this morning, there were more than 1800 people hospitalized, and over 450 in ICUs across the city. It is hard to imagine “the city that never sleeps” with near empty streets in the middle of the day; but the city has closed all non-essential businesses and gatherings, and most folks now seem to be taking it seriously. But there has been conflicting messaging from local, state and federal sources about the virus, and it has created an atmosphere of fear and confusion.
According to the New York Times, New York State has roughly 5% of coronavirus cases worldwide, and New York City, a disease epicenter, has over 25% of all COVID-19 patients in the US. As of this morning, there were more than 1800 people hospitalized, and over 450 in ICUs across the city. It is hard to imagine “the city that never sleeps” with near empty streets in the middle of the day; but the city has closed all non-essential businesses and gatherings, and most folks now seem to be taking it seriously. But there has been conflicting messaging from local, state and federal sources about the virus, and it has created an atmosphere of fear and confusion.
Beacon Christian Community Health Center, located on Staten Island, is living up to its name. Beacon is a Christ-centered FQHC, and a long-time member of the CCHF community. It’s founders, Drs. David and Janet Kim, were tailor-made for a situation like this. David is a med/peds doc with training in emergency preparedness; and Janet, also a med/peds doc, is trained in epidemiology. After Hurricane Sandy hit New York in 2012, the Kims played a significant role in setting up emergency medical care for Staten Island. They consulted other CCHF clinics after hurricanes Harvey and Irma, and have offered workshops on emergency preparedness. It is almost like they were born for this.
David & Janet Kim
“God has called us to be a beacon during this crisis. There is so much fear and misinformation out there. A big part of our role is to help people respect this virus, but not fear it.” I spoke at length with David Kim this morning. “Our numbers are down. Everyone’s numbers are down. There are times we are all humanly tired and concerned. But our phones are ringing off the wall with people who are terrified and panicking. It’s like everything they built their lives around is crumbling. I can’t tell you how powerful it is to share with them that God is still in control, and that He cares about them.”
David shared that during this crisis, there were three main roles they felt they were called to fulfill. First, they were to be a beacon to the people of New York – to be a visible pillar of truth and peace, helping them understand the facts in a way that empowers them and dispels fear. Second, they were to keep showing up, taking care of all of the things that people can’t go to the hospital for now. They are still providing full scope primary care, and making sure their patients have continuity of care. And third, they are deeply involved at the state and local level with the health departments and hospitals, facilitating reliable exchange of information and coordinated care. Through it all, they are dedicated to show and share the love of Jesus, pointing people to God as their source of security, life and peace.
I asked David about some ways this pandemic has impacted their work:
Their patient volume is down by approximately 25% due to increased no-shows, but they are still providing full service primary care.
About half of their patient encounters are in-office, and half are tele-medicine. That seems to be working pretty well. Tele-health visits with video for Medicaid patients are billable, and they hope that when Congress passes the relief bill this week that tele-health visits with Medicare patients will also be billable.
Their staff is doing well, in part because of clear protocols, systems and training that have been put into place, and in greater part because they are reminding each other that they are people whose faith in God and dedication to the mission is real and strong.
They have set up a dedicated space inside the clinic for patients who present with symptoms, have had exposure to someone with COVID-19, or have visited countries where there has been an outbreak of the virus. They are following CDC guidelines to the letter.
They find social media to be particularly critical in their work right now. Their social media presence and messaging has generated a lot of opportunities to stay in touch with their neighbors, to share helpful information, and has created a lot of ministry opportunities as they address anxiety and fear among their neighbors.
Prayer: Keep praying for their staff, and pray for them to remain faithful to their mission throughout this crisis. While others are running away from this disease, Beacon senses God's call to run towards it. Pray also for the financial, economic and other inevitable social challenges that will impact not only Beacon itself, but our underserved community, as well as the entire city, for a long time to come.
I appreciate David and the team at Beacon. They have always strived to love people well, and to respectfully and boldly share the hope we have in Christ. As we talked today, I was reminded that we help our patients and neighbors find inexplicable and unshakable peace when we direct them to take their anxieties to God in prayer (Philippians 4:6-7). That goes for us, too.
Let us know how this is impacting you and your clinic.
Stay safe. Be at peace.
In Christ’s love,
Steve Noblett